We know that everyone on an emergency care team is integral and valued. But our experience shows that nobody else has the training or expertise of an emergency physician.
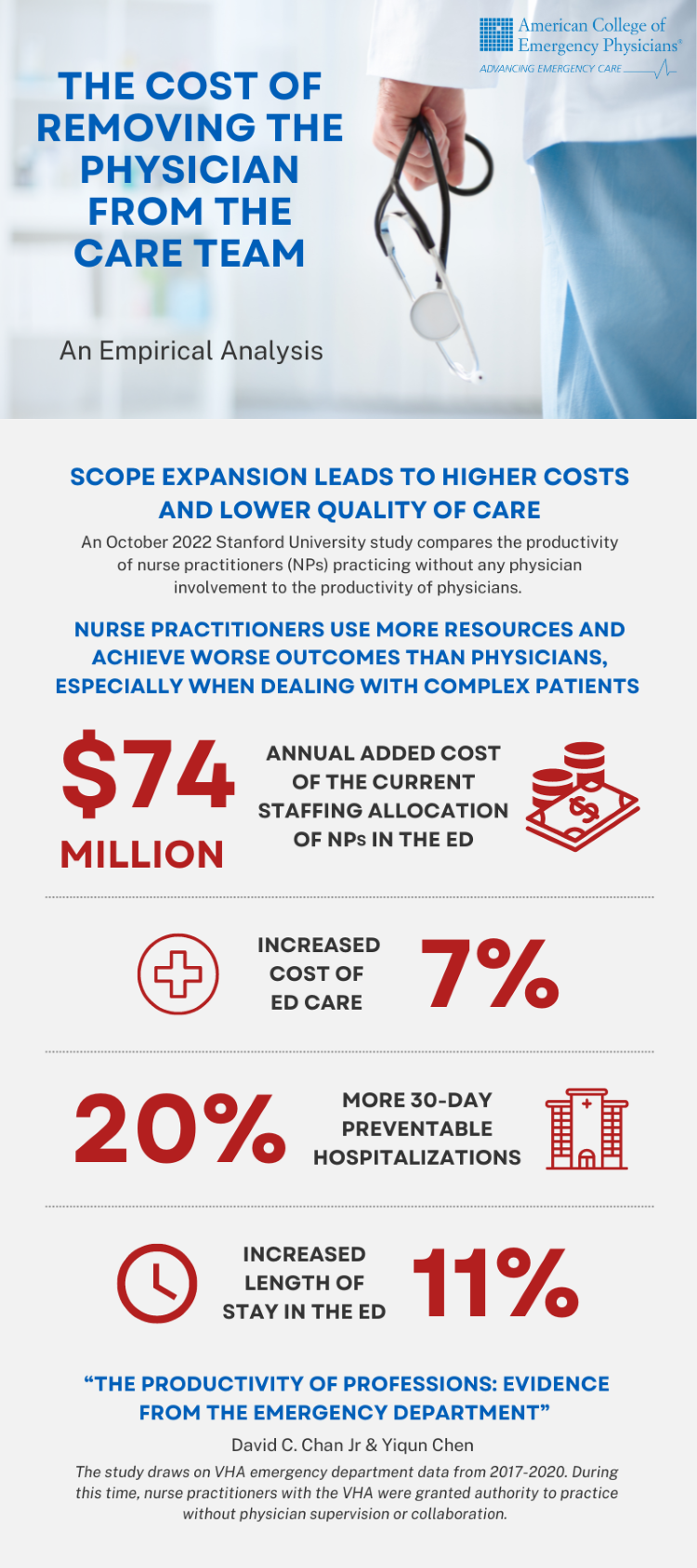
As lawmakers and administrators evaluate whether to empower nurse practitioners and physician assistants beyond the scope of their training, new data from Stanford University reinforces our reservations about exposing non-physician practitioners to responsibility they are not prepared to assume.
The Stanford study is uniquely strong because the researchers evaluated three years of data on emergency department visits at the Veterans Health Administration, where NPs were practicing without physician supervision. Unlike previous studies on the topic, this data was based on real world experience and the analysis is causal, not just correlative.
The study confirms that hiring NPs instead of physicians costs more money overall and results in worse outcomes, especially when dealing with complex patients.
Scope expansion can lead to higher costs and lower quality of care.
The study found that relying on unsupervised NPs led to unnecessary tests and procedures, and hospital admissions. Overall, the study shows that NPs increase the cost of care in the emergency department by 7%, about $66 per patient.
As the authors said, “differences in training may play some role in productivity differences between NPs and physicians.”
Lower productivity was the primary contributor to these increased costs—nurse practitioners were more likely than physicians to order x-rays, CT scans, and seek formal consults.
These choices also impact patient outcomes. NPs practicing without physician supervision increased length of stay in the emergency department by 11% and raised 30-day preventable hospitalizations by 20%, according to the study.
Advocating for Physician-Led Teams
This study adds compelling data that each of us can use to support advocacy based on our personal experience. We are hopeful that this new study helps lawmakers and administrators support physician leadership and prioritize policies that enhance the safety, quality, and efficiency of care.
ACEP is looking forward to leading a discussion about our advocacy work on physician-led care teams during the upcoming meeting of the American Medical Association’s Scope of Practice Partnership, which includes 105 national, state and specialty medical associations. We will continue to do all we can to make sure that legislators, hospital decisionmakers and others know that there is simply no substitute for a licensed and trained emergency physician in today’s complex clinical environment.