
The Perils of Abandoning the Pediatric FAST Exam
Antonio Riera, MD
Section of Pediatric Emergency Medicine, Department of Pediatrics
Yale-New Haven Children's Hospital, New Haven, CT
Yale University School of Medicine, New Haven, CT
In recent years, the pediatric focused assessment with sonography in trauma (FAST) exam has come under scrutiny. Critics argue that its diagnostic utility is limited, suggesting that its use should be reconsidered. However, abandoning the pediatric FAST exam would be a premature and potentially dangerous decision. Our experience suggests that maintaining and improving this vital diagnostic tool is crucial to enhance pediatric trauma-informed care.
Outdated Test Characteristics
The primary criticism against the pediatric FAST exam is that it has poor sensitivity for the detection of hemoperitoneum. This data was derived in the 1990s and has become outdated as ultrasound technology rapidly advances; newer machines offer better resolution and imaging capabilities, which can significantly enhance diagnostic accuracy. New studies to reassess the effectiveness of the FAST exam using the latest technology are necessary. Relying on outdated data not only misrepresents the current capabilities of the exam but also hinders its potential benefits in pediatric trauma care.
Seeing More than Just Free Fluid
Recent cases at our hospital highlight the enhanced diagnostic potential of the FAST exam, thanks to advancements in ultrasound image quality.
Case 1
A 13-year-old male suffers a handlebar injury to the left upper quadrant while riding a bicycle. He is brought to the emergency department by ambulance with stable vital signs and is initially evaluated in a hallway bed. He has abdominal pain and a circular abrasion on the left upper abdomen. A FAST exam reveals hemoperitoneum in the pelvis and signs of splenic rupture, and he is promptly moved to the major treatment room. The spleen loses its normal homogeneous gray echotexture. Instead, areas of increased echogenicity (brightness) due to acute edema are juxtaposed with hypoechoic ragged linear lacerations (Video 1). A computed tomography (CT) scan confirms a grade 4 splenic laceration. The patient is hospitalized for 48 hours and does well with non-operative management. A few days after discharge, he returns with a new fever, ongoing abdominal pain, and a cough. A repeat FAST exam reveals no progression of intra-abdominal fluid but a new development of a pleural effusion on the left side (Video 2). Lung tissue hepatization is present with dynamic air bronchograms (Video 3). A dedicated view of the spleen reveals persistent signs of tissue injury (Video 4). He is treated with high-dose amoxicillin for bacterial pneumonia and fully recovers on a follow-up visit.
Case 2
A 2-year-old male suffers multi-system trauma after accidentally being run over by a car. He is brought to the pediatric emergency department within half an hour. Vital signs are notable for tachycardia. The patient is intubated due to signs of significant head trauma and a low Glasgow coma score. On FAST examination, the bladder is not visible, and there is no free fluid. However, there is abnormal-appearing liver echotexture suggestive of a laceration injury (Video 5). A CT scan confirms a high-grade liver laceration.
Case 3
A 14-year-old male suffers a handlebar injury to the lower left abdomen after a fall from a bicycle. His vital signs are normal. On physical exam, there is a circular imprint in the left lower quadrant (Figure 1). His abdomen is soft with mild tenderness to palpation. On FAST examination, there is free fluid in the pelvis. Additional images over the area of impact reveal an abdominal wall defect with signs of a traumatic bowel hernia (Video 6). The intestine can be seen crossing the fascial plane into the soft tissue. A CT scan confirms the disruption of the abdominal musculature fascia in the left lower quadrant. The patient requires laparoscopy to identify and repair the defect (Figure 2)
Figure 1
Figure 2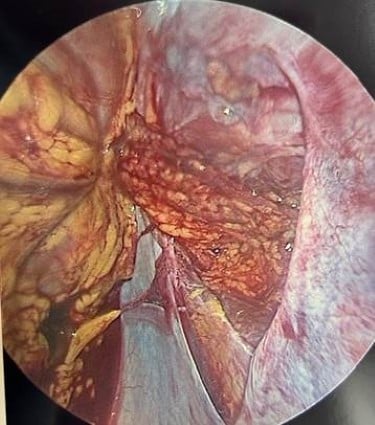
Case 4
A 16-year-old male presents with acute hematuria and abdominal pain after being checked with a lacrosse stick during practice. He is hemodynamically stable with a heart rate of 58. A FAST exam is performed by the treating clinician within 15 minutes of arrival to the pediatric emergency department. On FAST examination, there is free fluid in the right upper quadrant, and a mass is visible at the edge of the liver where the kidney is expected to be seen (Video 7). On the suprapubic view, the bladder contains a large echogenic clot (Video 8). Immediate surgical consultation and a CT scan confirm the presence of a large retroperitoneal hematoma with extravasation (Figure 3). The patient requires urgent operative intervention and nephrectomy.
Figure 3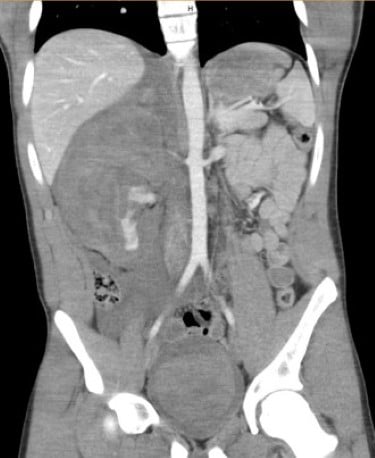
These four cases highlight the critical role of newer ultrasound technology in the careful evaluation of traumatic injuries in pediatric patients. Initially designed to detect free fluid, the FAST exam in each of these cases reveals additional injuries, thanks to image resolution enhancements of newer devices.
Case 1 demonstrates how POCUS was able to detect hemoperitoneum and splenic laceration, guiding prompt management on initial presentation. On representation for worsening symptoms, POCUS was able to identify subsequent complications such as a pleural effusion and pneumonia, avoiding unnecessary and harmful radiation.
Case 2 illustrates the use of FAST to identify a liver laceration in a young child with multi-system trauma, even when free fluid was not present, underscoring its potential future value in evaluating solid organ injuries.
Case 3 shows how detailed imaging can reveal an abdominal wall defect and traumatic bowel hernia, facilitating timely surgical intervention.
Case 4 emphasizes the FAST exam's ability to detect complex injuries, such as a retroperitoneal hematoma and a bladder clot, leading to life-saving surgical treatment.
Together, these cases underscore the importance of recognizing that with current advancements in ultrasound technology for pediatric trauma care, the detection of injuries beyond the initial scope of the FAST exam is possible. In addition, the rapid findings obtained by performing the FAST exam expediated care, provided confidence in the need to obtain CT scans and surgical consultations, and helped alleviate the cognitive burden associated with disposition and other timely management decisions.
The Evolution from Diagnostic Peritoneal Lavage
The FAST exam has effectively supplanted diagnostic peritoneal lavage (DPL) as the preferred method for bedside evaluation of hemoperitoneum in trauma patients. Historically, DPL was a standard procedure involving the invasive insertion of a catheter into the peritoneal cavity to detect internal bleeding. While effective, DPL carried risks such as infection and injury to internal organs. The advent of the FAST exam revolutionized trauma assessment by offering a non-invasive, rapid, and accurate alternative for detecting free fluid indicative of internal bleeding. Enhanced ultrasound technology and the growing expertise of pediatric emergency physicians in POCUS have further solidified the FAST exam's role. This shift has not only minimized patient risk but also streamlined trauma care, allowing for quicker, safer, and more efficient diagnosis of severe intra-abdominal hemorrhage typically caused by high grade liver or splenic lacerations. The replacement of DPL with the FAST exam exemplifies the ongoing advancement in medical practices, prioritizing patient safety and diagnostic accuracy.
Unfair Comparisons with CT Scan Utilization
Critics often use CT scan utilization rates as a benchmark to judge the effectiveness of the FAST exam. However, this comparison is fundamentally flawed. The FAST exam and CT scans answer different clinical questions and serve different purposes. When considering the assessment of acute appendicitis - if we were to randomize physicians such that some had access to CBC results and others did not and found that there was no difference in the rate of acquiring an appendix ultrasound between these groups, it would be erroneous to conclude that a CBC is unnecessary in diagnosing appendicitis. The preponderance of evidence and clinical decision rules use a total white blood cell count and percentage of neutrophils as objective variables to risk stratify children for the diagnosis of acute appendicitis. Similarly, the goal of the FAST exam is not to replace CT scans but to serve as an initial, rapid assessment tool that can guide further diagnostic steps. A positive FAST with more than physiological quantities of free fluid should expedite CT scan to rule out high grade liver and spleen lacerations or other associated injuries. A negative FAST should alert the clinician to consider retroperitoneal or hollow viscous trauma, if a pediatric blunt abdominal trauma patient remains clinically symptomatic with abdominal tenderness on serial exams. Judging the FAST exam solely by its impact on CT scan utilization overlooks its broader clinical utility and the nuanced role it plays in pediatric trauma care.
The Impact of Expertise on Performance
The accuracy and effectiveness of the FAST exam are significantly influenced by the expertise of the practitioner performing it. In pediatric settings, where POCUS (point-of-care ultrasound) expertise exists, there is tremendous potential for improvements by non-experts. As more pediatricians gain experience and training in POCUS, the diagnostic performance of the FAST exam is likely to improve. Dismissing the FAST exam now, without allowing for this gradual enhancement in skill and expertise, would be a disservice to its future potential. Investments in training and standardizing pediatric POCUS can elevate the performance and reliability of the FAST exam, making it an indispensable tool in trauma care.
Lack of Multicenter Studies and a Role for P2 Network Participation
One of the significant gaps in the current research landscape is the absence of large, multicenter studies conducted by pediatric emergency medicine POCUS experts. The P2 Network is the premier group of specialists in pediatric POCUS, and their involvement in research is crucial for producing high-quality, generalizable data. Their expertise and coordinated efforts could provide the robust evidence needed to validate and refine the pediatric FAST exam. Until such studies are undertaken, any move to abandon the FAST exam is premature and not based on sufficient evidence.
The Importance of Allocating Resources to Training
Dedicating resources to training for the FAST exam is crucial, particularly given the relatively rare occurrence of abnormal findings in pediatric blunt abdominal trauma, estimated at about 5-10% in one study at a tertiary care children’s hospital.1 Trainees must master the identification of normal anatomy and how to troubleshoot image acquisition to accurately detect abnormalities. Research indicates that an average learner needs to review approximately 90 cases to achieve a performance benchmark of 90% accuracy in image interpretation.2 This underscores the necessity of dedicated teaching time for novice ultrasound users, especially those who provide essential trauma care. Ensuring that trainees receive comprehensive and rigorous training enables them to reach their full potential, ultimately improving the quality of care for pediatric trauma patients. Investing in this education not only enhances diagnostic accuracy but also contributes to better patient outcomes and more efficient use of medical resources.
Conclusion
Abandoning the pediatric-focused FAST exam overlooks the significant advancements in technology, the unique role it plays in trauma assessment, the potential for improved accuracy with increased expertise, and the need for high-quality research from leading experts. Rather than discarding this valuable diagnostic tool, we should focus on updating its data, enhancing physician training, and conducting robust multicenter studies. By doing so, we can ensure that the FAST exam remains a vital component of pediatric informed-trauma care, with great potential to improve outcomes for our youngest patients.
References
- Riera A, Hayward H, Silva CT, Chen L. Reevaluation of FAST Sensitivity in Pediatric Blunt Abdominal Trauma Patients: Should We Redefine the Qualitative Threshold for Significant Hemoperitoneum? Pediatr Emerg Care. 2021;37(12):e1010-e1019.
- Kwan C, Weerdenburg K, Pusic M, Constatntie E, et al. Learning Pediatric Point-of-Care Ultrasound: How Many Cases Does Mastery of Image Interpretation Take? Pediatr Emerg Care. 2022;38(2):e849-e855.

