PEM Pocket Card: Intussusception
Lindsey Chaudoin MD
Carolinas Medical Center
Case
A 26-month-old male presented to the emergency department at 11pm for ongoing abdominal pain for 2 days. His parents noted that he initially seemed to be eating less and having difficulty with bowel movements. He had had no stool since the day prior and was seen in urgent care and started on MiraLAX for constipation. On morning of presentation, he started vomiting and seemed more uncomfortable. He had no fevers or cough at home but is febrile and mildly tachycardic on presentation.
The provider performed a bedside US of the abdomen to evaluate for signs of obstruction and free fluid. By using graded compression in the “picture frame technique” to assess the colon, the provider was able to identify a target shaped 2.5 cm tissue density at the hepatic flexure consistent with ileocolic intussusception. Radiology was notified and the radiologist mobilized the IR suite for reduction.
Technique
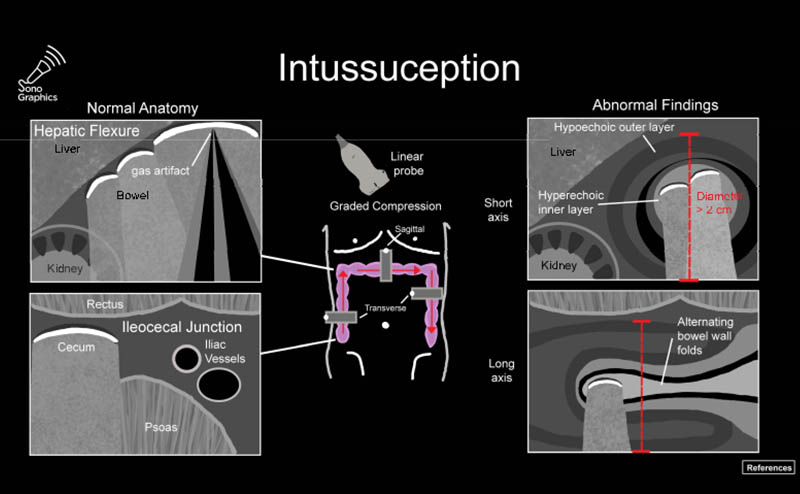
The linear probe is placed in the RLQ in the transverse position with indicator to the patient’s right. Identify the psoas muscle and iliac vessels lying medial. Once these structures are visualized, slide lateral and look superficially to identify the cecum. (Figures 1a,1b 1) Use graded compression-progressive increase and decrease of pressure to move any gas out of view. Keeping the lateral edge of the abdominal cavity in view (Figure 2), the ultrasound probe should slide cranial in traverse plane, visualizing the ascending colon until the hepatic flexure. In this location, the colon turns just medial to the liver with the kidney deep in the view. (Figure 3) This is the most common location to identify ileocolic intussusception. If no tissue mass is identified, the probe should be turned to the sagittal plane with indicator toward the head (to keep the colon visualized in the transverse view) and moved across the transverse colon continuing to use graded compression to look for a tissue mass consistent with intussusception. Once at the splenic flexure (Figure 4), the probe should be transitioned back to the transverse orientation to interrogate the descending colon.
The abnormal structure of intussusception is a rounded tissue mass in the transverse axis with a hyperechoic center and hypoechoic outer muscle layer (Figure 5) and in long axis appears as a “pseudokidney.” (Figure 6) Outer dark edge to edge should be at least 2cm.1-3 Smaller structures with similar appearance are likely ileo-ileal intussusception, which is usually psychologic and does not typically require intervention.
Outcome
The intussusception was successfully reduced in radiology with an air enema. The patient returned to the emergency department where he tolerated PO and remained comfortable for several hours and was discharged home.
Discussion
Intussusception is a medical emergency in which one part of the intestine invaginates into a more distal part of the intestine, causing an intestinal obstruction. In severe cases, this can lead to bowel perforation, sepsis and death. The invaginating tissue creates a tissue mass without gas in the large intestine, and this path is predictable in location in the abdomen. These factors allow ultrasound to be the diagnostic modality of choice for intussusception, and has been shown to have high accuracy both by radiology4 and at the bedside.1,5,6 Identification of the intussusception by point of care ultrasound streamlines care for pediatric patient in several ways. For the provider, it rapidly narrows the differential when positive to limit the workup to the appropriate diagnosis and allows the provider to mobilize the patient for treatment or transfer and move on to other patients in the department. For the patient, identifying the pathology quickly allows shorter delays in getting the patient to ultimate reduction. Given the predictable location of the colon, if a provider can master the skills of graded compression, POCUS for intussusception is a highly accurate application that is not difficult to learn.
To help with remembering the technique and measurement requirements for pediatric applications, the Pediatric Subcommittee and the Critical Care Subcommittee of ACEP Emergency Ultrasound have created PEM POCKET cards, including one for intussusception. See Figure 7, and access the other cards at ACEP PEM Pocket Cards.
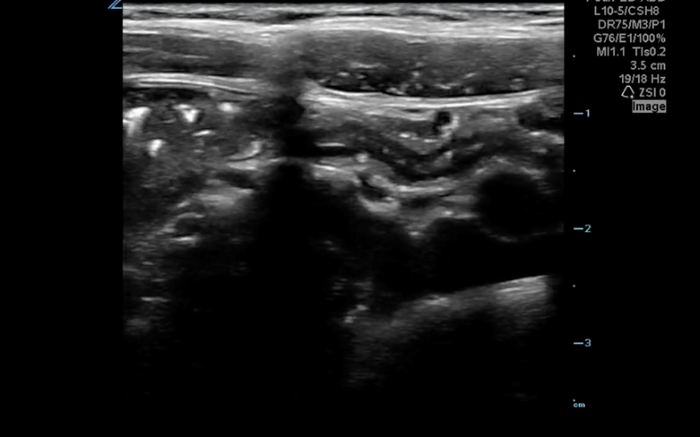 Figure 1a. Unlabeled anatomy of identifying landmarks of RLQ to identify cecum.
Figure 1a. Unlabeled anatomy of identifying landmarks of RLQ to identify cecum.
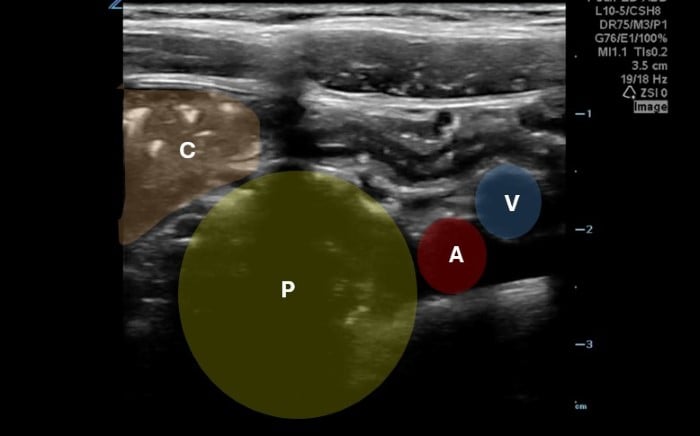 Figure 1b. Right lower quadrant anatomy: A-iliac artery, B-iliac vein, P-psoas muscle, C-cecum of identifying landmarks of RLQ to identify cecum.
Figure 1b. Right lower quadrant anatomy: A-iliac artery, B-iliac vein, P-psoas muscle, C-cecum of identifying landmarks of RLQ to identify cecum.
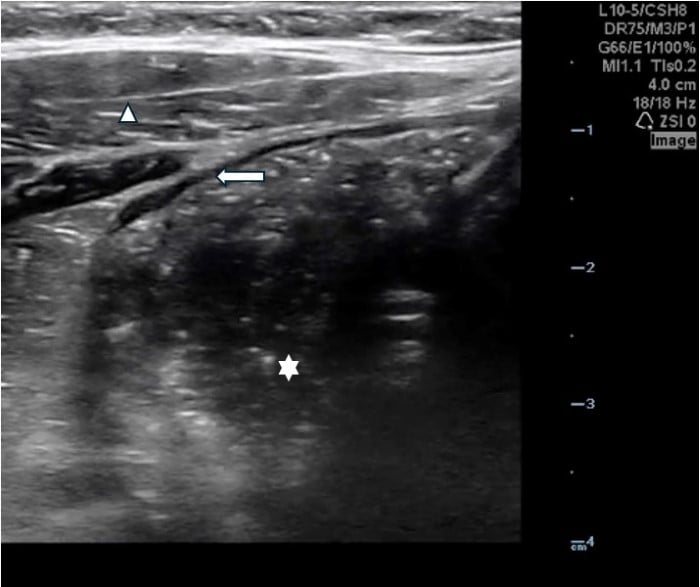 Figure 2. Lateral border of right abdomen maintained in view with “starry night” appearing stool in colon (white star), transverse abdominus muscles (triangle) and border of the peritoneal cavity (white arrow)
Figure 2. Lateral border of right abdomen maintained in view with “starry night” appearing stool in colon (white star), transverse abdominus muscles (triangle) and border of the peritoneal cavity (white arrow)
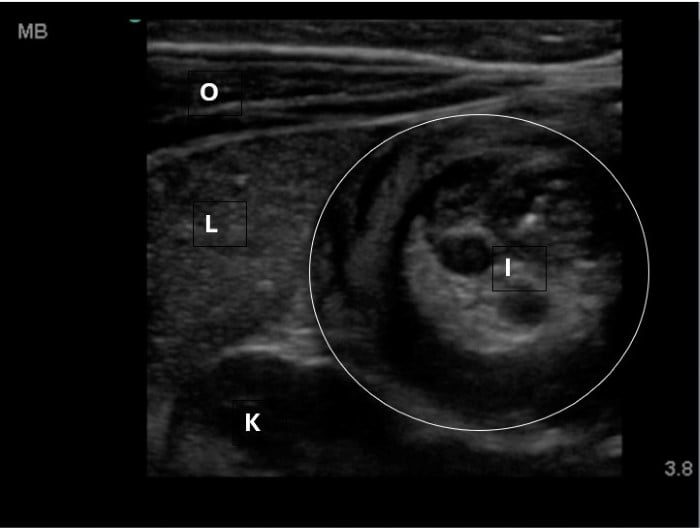 Figure 3. Hepatic flexure view in a patient with intussusception. Oblique abdominal muscles, liver, kidney visible. Intussusception will be medial to the liver and superficial to the kidney.
Figure 3. Hepatic flexure view in a patient with intussusception. Oblique abdominal muscles, liver, kidney visible. Intussusception will be medial to the liver and superficial to the kidney.
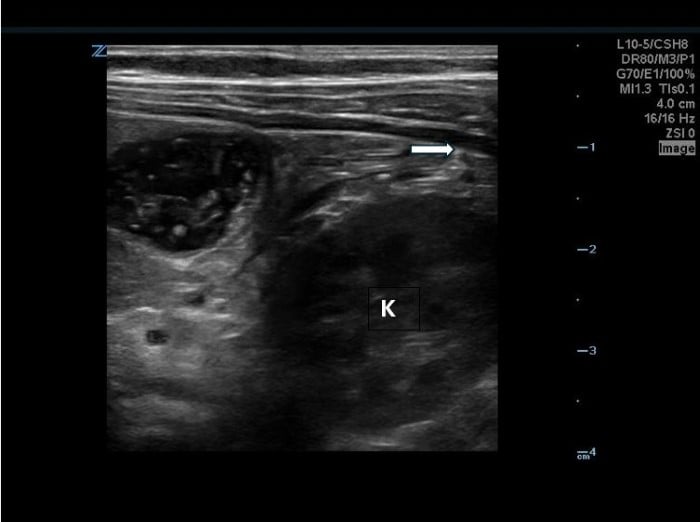 Figure 4 LUQ Colon perimeter with kidney and edge of peritoneum in view.
Figure 4 LUQ Colon perimeter with kidney and edge of peritoneum in view.
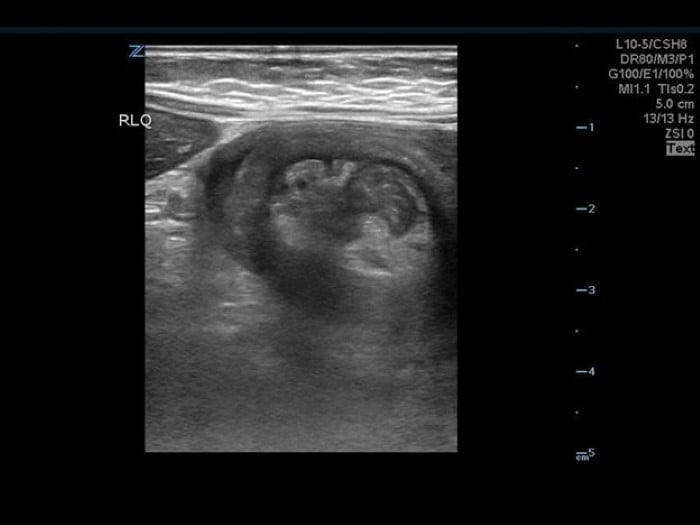 Figure 5. Short axis view of intussusception. Note the hyperechoic center and the hypoechoic outer layer, and the liver lying lateral.
Figure 5. Short axis view of intussusception. Note the hyperechoic center and the hypoechoic outer layer, and the liver lying lateral.
 Figure 6. Long axis Intussusception, sometimes referred to as the “Pseudokidney” as it mimics the kidney’s shape in sagittal.
Figure 6. Long axis Intussusception, sometimes referred to as the “Pseudokidney” as it mimics the kidney’s shape in sagittal.
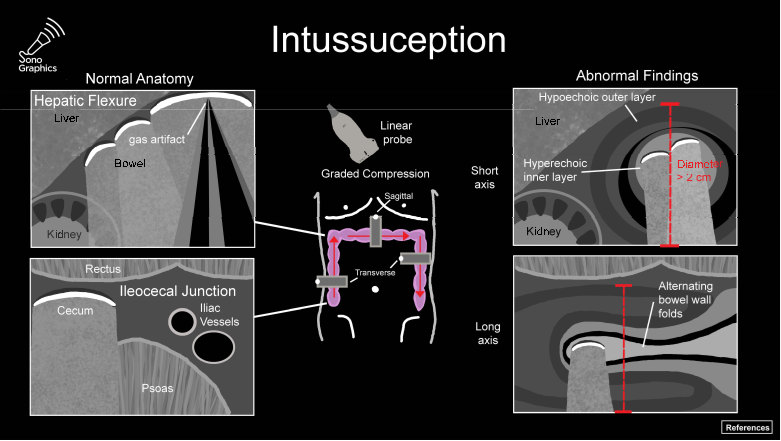 Figure 7. Peds Pocket Card for Intussusception
Figure 7. Peds Pocket Card for Intussusception
References
- Bergmann KR, Khant M, Lammers S, et al. Accuracy and Interrater Reliability of Point-of-Care Ultrasonography Image Interpretation for Intussusception. Pediatr Emerg Care. 2022;38(9):442-447.
- Wiersma F, Allema JH, Holscher HC. Ileoileal intussusception in children: ultrasonographic differentiation from ileocolic intussusception. Pediatr Radiol. 2006;36(11):1177-1181.
- Kim JH. US features of transient small bowel intussusception in pediatric patients. Korean J Radiol. 2004;5(3):178-184.
- Hryhorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009;39(10):1075-1079.
- Riera A, Hsiao AL, Langhan ML, Goodman TR, Chen L. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med. 2012;60(3):264-268.
- Lin-Martore M, Kornblith AE, Kohn MA, Gottlieb M. Diagnostic Accuracy of Point-of-Care Ultrasound for Intussusception in Children Presenting to the Emergency Department: A Systematic Review and Meta-analysis. West J Emerg Med. 2020;21(4):1008-1016.

