POCUS on the Peds Side: A World of Its Own
Chris Lumpkin, MD
Emory University

Point-of-care ultrasound (POCUS) has been a topic of great interest, debate, and promise over the last few decades. Applications in pediatrics go back as far as the 1980’s while in 1990 ACEP published its first position statement on the topic with a pediatric statement not to follow until 2014.1,2,3 Since then, the field has grown while wrestling with the complex task of not only identifying the best use of the technology in pediatrics as a whole but leveraging unique considerations that come from changing patient size and epidemiology. With that, training has commensurately grown to match as new generations of trainees graduate with increasing comfort and competency, while definitions of competency itself continue to evolve.4 POCUS is ideally suited to pediatric care which can present multiple challenges including inconsistent 24 hours specialized imaging support, a population often unable to communicate their symptomatology, and the added importance of limiting radiation exposure
Figure 1. Intussusception “pseudokidney sign” described on pediatric patient in 2009
As with other applications and technologies, the pediatric population poses not only the opportunity to learn directly from adult approaches, but to also both recognize unique pediatric techniques and uncover some that benefit our adult colleagues in kind. With these goals in mind, research has been ongoing while institutions do their best to synthesize decades of experience in neighboring specialties to determine how to safely and effectively implement POCUS at their institutions. There are numerous online resources aiming to fill the gap currently existing in the certification space for POCUS in pediatric subspecialties, but few are universally accepted by their specialties. Further complicating this is that institutional and specialty needs will vary. Hours of coursework will possibly take one past basic competency in one discipline and only the beginning in another. The prospect of additional fellowship training with minimum 3 year pediatric fellowships and no guarantee of a compensation structure for ultrasound directorship is daunting with implications for growing expertise and acquisition of advanced skill sets. This leaves training on the job with local support supplemented by varied local and national offerings to fill those gaps with strains on time by clinical demands.4
“[This] makes it difficult to get people enough clinically-relevant scanning experience to be able to comfortably identify pathology and feel confident using POCUS in some of those rarer but high stakes critically-ill patients”- Matthew Moake MD, PhD MUSC
“Given the relative paucity of POCUS trained [attendings] at most institutions, trainees don’t consistently get encouragement to perform POCUS as part of their routine patient care”- Russ Horowitz MD, Lurie Children’s
And even with more and more resources helping spread education, the actual work of running a program faces the same funding hurdles that affect pediatrics as a whole. Finding ways to justify middleware purchases and clinical time for quality assurance (QA) has been an obstacle and often overcome after years of sweat-equity. To this end, motivated individuals and groups have made tremendous progress towards robust QA infrastructure using non-middleware solutions, while others through partnering with other divisions have joined to make third party middleware a possibility at their institutions.
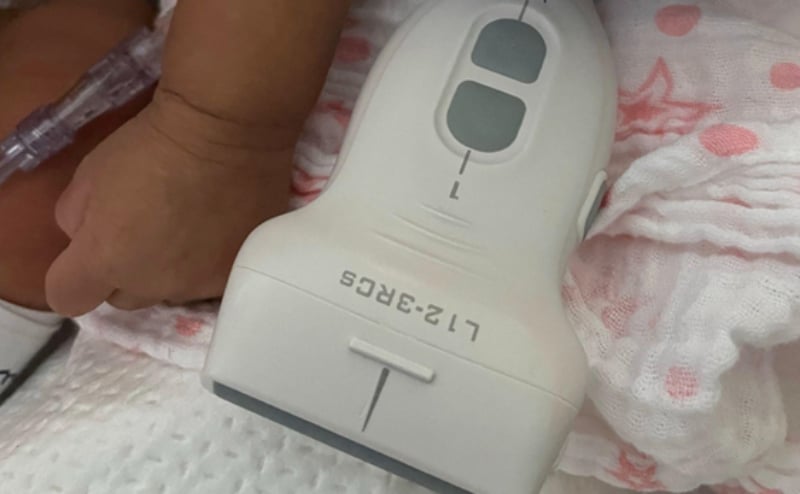
None of this has prevented the development of more distinct adaptations of POCUS for the pediatric population. Unique applications in children have included infant lumbar punctures guided by direct visualization of the cauda equina, protocols for intussusception, algorithms to confirm endotracheal tube placement, and the expansion of ultrasound first approach to appendicitis among many more yet at bedside. Bedside experience coupled with research has uncovered unique advantages our smaller patients offer in regard to image depth and clarity for structures not well imaged in adults. As a result, what has followed includes specific probe advancements allowing access to higher frequency and smaller footprints. This has allowed visualization of submillimeter neonatal vasculature and the ability to peer between infant ribs and tailor neonatal presets.
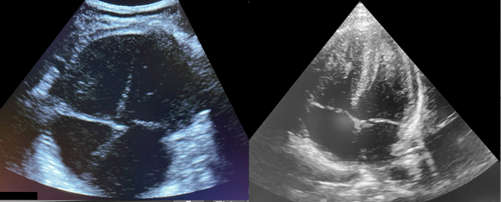
Figure 2. Comparison of an adult microconvex probe set to adult cardiac preset (L) and neonatal phased array probe set to neonatal Preset (R)
In addition to these advancements already coming into practice, progress continues to be made in finding novel ways to limit the need for radiographs or unnecessary procedures. At any conference covering the topic, one can hear about evaluation for esophageal foreign body, infant skull fractures, diagnosing distal limb fractures, and a multitude of other applications representing an energized community discovering and defining the age-old same-but-different physiology in pediatrics with ultrasound.6,7,8

Figure 3. Conus medullaris visualized in long axis prior to lumbar puncture in infant
When soliciting opinions for this piece, the breadth of experiences and attitudes was broad, but not surprising. As with the differences in so many facets of patient care, the path toward POCUS acceptance, skills, practical integration, and collaboration has not just been different from our adult peers but across divisions and institutions. As detailed above, these differences make the growth of POCUS in pediatrics that much more exciting. The pediatric POCUS community continues to forge forward and carve out a niche in the broader conversations on how bedside ultrasound fits into and enhances current standards of care for our vulnerable patients.
All images obtained with consent from parents or referenced source below.
References
- Marin JR, Lewiss, RE. American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, Society for Academic Emergency Medicine, Academy of Emergency Ultrasound, American College of Emergency Physicians, Pediatric Emergency Medicine Committee, World Interactive Network Focused on Critical Ultrasound, ... & Volpicelli, G. Point-of-care ultrasonography by pediatric emergency medicine physicians. Pediatrics. 2015;135(4), e1113-e1122.
- Shkolnik A, Foley MJ, Riggs TW, & Devine S. New application of real time ultrasound in pediatrics. 1982;2(3):422-36.
- Kairam N, Kaiafis C, Shih R. Diagnosis of pediatric intussusception by an emergency physician-performed bedside ultrasound: a case report. Pediatr Emerg Care. 2009;25(3):77-180.
- Marin JR, Zuckerbraun NS, Kahn JM. Use of emergency ultrasound in United States pediatric emergency medicine fellowship programs in 2011. J Ultrasound Med. 2012;31(9):1357-63.
- Kutanzi KR, Lumen A, Koturbash I, Miousse IR. Pediatric exposures to ionizing radiation: carcinogenic considerations. Int J Environ Res Public Health. 2016;13(11):1057.
- Buonsenso D, Chiaretti A, Curatola A, Morello R, Giacalone M, Parri N. Pediatrician performed point-of-care ultrasound for the detection of ingested foreign bodies: case series and review of the literature. J Ultrasound. 2021;24:107-14.
- Alexandridis G, Verschuuren EW, Rosendaal AV, Kanhai DA. Evidence base for point-of-care ultrasound (POCUS) for diagnosis of skull fractures in children: a systematic review and meta-analysis. Emerg Med J. 2022;39(1):30-6.
- Snelling PJ, Jones P, Bade D, Bindra R, Davison M, Gillespie A et al. Diagnostic Accuracy of Point-of-Care Ultrasound Versus Radiographic Imaging for Pediatric Distal Forearm Fractures: A Randomized Controlled Trial. Ann Emerg Med. 2024;83(3):198-207.