
Cerebral Air Embolism Treated With Hyperbaric Oxygen Therapy
Mason Gay, MD; Drue Orwig, DO, MBA, CWSP
Corewell Health - Michigan State University Emergency Medicine Residency Program, Grand Rapids Michigan
Introduction
An air embolism occurs when a pocket of air enters the vasculature. They can range clinically from only mild symptoms to debilitating or lethal.6 While rare, Air embolisms can be catastrophic if they reach cerebral arterial vasculature or by impairing cardiac output.4 When presenting with neurologic deficits, air emboli are commonly misdiagnosed as a thrombotic stroke.3 They can arise due to barotrauma such as divers surfacing too quickly, penetrating trauma, or iatrogenically as a known complication to procedures performed both in the inpatient and outpatient setting. Despite the infrequency of this phenomenon, hyperbaric oxygen therapy (HBOT) has shown in limited studies to be an effective treatment. Hyperbaric oxygen for treatment of arterial emboli is currently an American Heart Association class 1 recommendation with level C evidence. HBOT for management of an air embolism is based upon the principle of Boyle’s Law that states that the pressure and the volume of a gas have an inverse relationship. If pressure on an air embolus is increased, then its volume will decrease.5 HBOT can also block the ischemia-reperfusion injury that can occur as blood flow through the artery returns. Literature suggests that the sooner HBOT is initiated the better the outcome.1,2 It is important for emergency physicians to be familiar with this topic, so that it can be appropriately recognized and managed in a timely manner. However, it is also worth stating that even with immediate recognition of an air embolism a barrier to care exists in that there are limited resources to provide HBOT. In the state of Michigan where this case presented, there are only two accredited clinical hyperbaric medical facilities (uhms.org) and only one that accepts emergent cases. This report will describe a case of an iatrogenic cerebral arterial air embolism that presented to the emergency department with significant neurologic deficits and was successfully managed with hyperbaric oxygen therapy.
Description of the Case
A 36-year-old female with relevant past medical history that included obesity, migraines, prior isolated seizure in 2010 among other comorbidities who had presented to the emergency department via EMS as a code stroke activation. Patient received an outpatient injection of sodium tetradecyl sulfate for sclerotherapy of varicose veins via vascular surgery. This procedure uses a foam mix of CO2:O2 and sodium tetradecyl sulfate injected into the varicose vein. A venous air embolism is a very rare complication of this procedure. This patient had the sclerotherapy injection around 1555 then around 1600 started complaining of a headache, weakness, and was noted to have slurred speech. On arrival to the emergency department, patient was found to have dysarthria, left-sided facial weakness, gaze deviation to the right, left arm and left leg near flaccidity, and left sided sensory deficits. She had a total NIH stroke scale score of 19. She had a GCS 15, and was awake and alert and able to answer questions appropriately to assist with history. Patient denied any trauma, recent illness, chest pain, shortness of breath, or abdominal pain.
Initial objective data included T 37C, HR 85, RR 20, BP 153/109, spO2 98%. Glucose 102. Basic labs obtained and were unremarkable. Patient was rapidly taken to CT for stroke imaging. No contraindications to thrombolytics were identified. At 1708, noncontrast head CT showed no hemorrhage, but an abnormal hypodensity along the right middle cerebral artery concerning for an air embolus was visualized. CT angiogram head and neck was also suggestive of air embolus and CT perfusion brain demonstrated 27 mL of critical hypoperfusion at the right posterior middle cerebral artery distribution.
It was then determined that the patient would not benefit from thrombolytics but would potentially benefit from hyperbaric oxygen therapy. Hyperbaric oxygen team was consulted to arrange urgent therapy and HBOT initiated at 1814 with plans for a US Navy Table 6 treatment. Approximately halfway through treatment, patient felt a “pop” and began to regain neurologic function after this and was noted to have “near resolution” of neurologic symptoms following initial US Navy Treatment Table 6 without extensions. Patient did endorse continuing to have tingling of the L hand and foot with pressure on follow-up exam the next day. She had one additional US Navy Table 5 treatment. TEE later performed which showed large atrial septal defect with bidirectional shunting. Patient eventually discharged to home with normal neurologic exam. She was later readmitted for an elective atrial septal defect repair with Cardiothoracic Surgery.
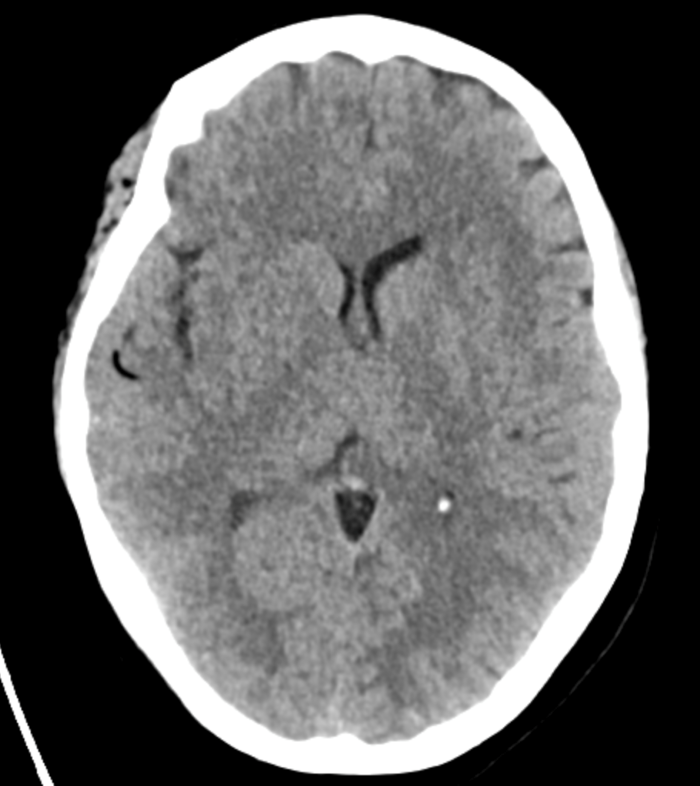
Figure 1: Non contrast Head CT showing air in the R MCA distribution
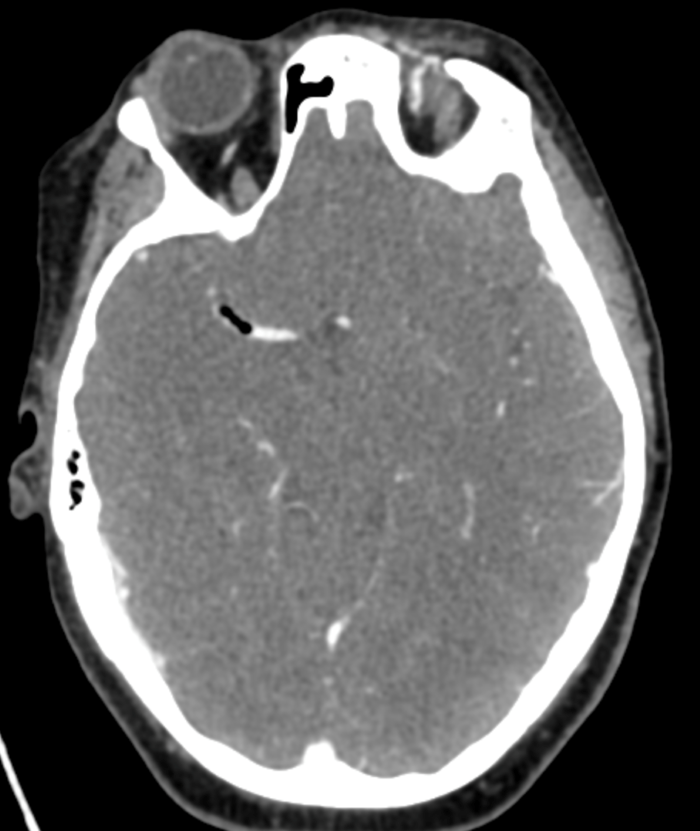
Figure 2: CT angiogram Head/Neck showing air in the R MCA
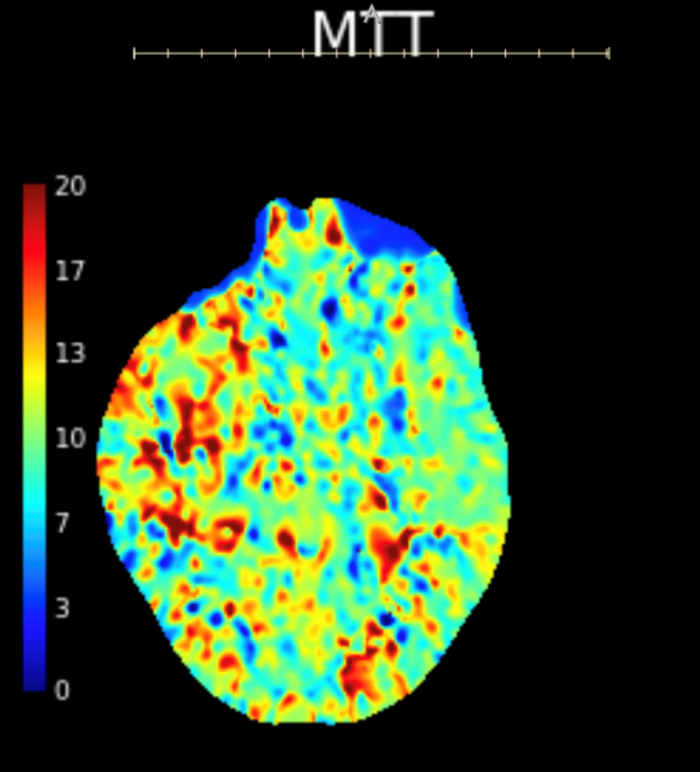
Figure 3: CT perfusion brain showing prolonged mean transit time in the right MCA distribution compared to the left MCA.
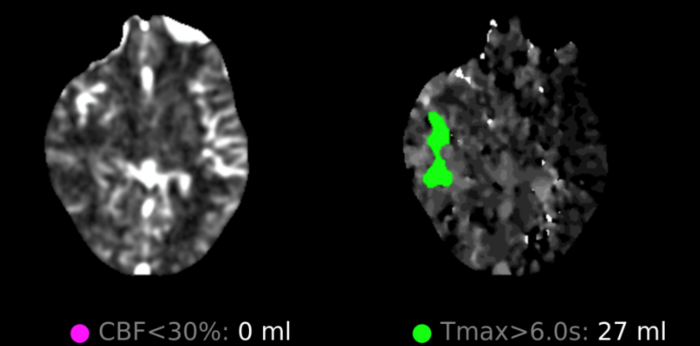 Figure 4: CT perfusion brain showing calculated 27 ml area of critical hypoperfusion with >6 seconds time-to-maximum filling.
Figure 4: CT perfusion brain showing calculated 27 ml area of critical hypoperfusion with >6 seconds time-to-maximum filling.
Discussion
Cerebral air embolism is a rare cause of brain hypoperfusion and neurologic deficits. These embolisms can cause profound neurologic deficits and timely management is of the utmost importance. Literature suggests outcomes are best the earlier HBOT is initiated and ideally within 6 hours of symptom onset 1, 2. Although there is some literature on the topic, more work is still needed. Studies are limited for a number of reasons such as the low incidence of cases, few centers that can do emergent hyperbaric treatments, and due to ethical concerns over withholding HBOT in a control group for any potential randomized controlled trials. In this case, HBOT was started approximately 2 hours and 14 minutes after symptom onset and led to a good outcome with near resolution of symptoms after presenting with severe deficits. Also consistent with prior retrospective work, this patient was later found to have a structural atrial septal defect allowing for an embolism to easily travel from R to L cardiac circulation. A study by McCarthy found 77% of patient with a cerebral air embolism who received an echocardiogram were found to have similar heart defects4. At first thought, one might expect that the number of cardiac defects to be 100%. Another paper explains how a venous air embolism can still reach cerebral arterial circulation without a structural shunt defect. Although pulmonary arterioles and capillaries can effectively filter out fat and clots, air passes through the lungs more easily5. This allows air emboli to still travel through the lungs to reach systemic circulation instead of needing to bypass the lungs through a heart defect like a fat or thrombotic embolus.
As mentioned previously, literature suggests that the earlier HBOT is initiated then the better the outcomes. However, there are significant barriers to starting therapy early. First, these cases are rare. While the total incidence of cases is not well documented, a study at a large tertiary care center only identified 6 cases over a 21-year period3. A systemic review published in 2023 researching air embolisms looking for any study published in English only found a total number of 263 well studied cases2. With the low incidence of cases, it is likely not a pathology that physicians retain a high index of suspicion for and not something that all emergency physicians, neurologists, or radiologists are going to be familiar with identifying and managing. A second barrier to early therapy is the availability of facilities with this capability. The Undersea and Hyperbaric Medical Society has a complete list on their website of U.S accredited clinical hyperbaric medical facilities (uhms.org). In the state of Michigan where this case presented, there are only 2 such facilities and only 1 of those 2 can accept emergent cases. Fortunately, this patient presented to the one center that had this emergent treatment available. In some states, the ability to do emergent hyperbaric treatment may require a flight to another state or region that offers emergent treatments.
Conclusion
This is a case of a cerebral arterial gas embolism that developed following an outpatient vein procedure and initially presented to the emergency department with severe neurologic deficits. Air emboli are a known but rare complication of many medical procedures. They can be managed with hyperbaric oxygen therapy and research has shown that the sooner this treatment is started then the better the outcomes. In this case, HBOT was started a little over 2 hours after symptom onset and the patient had near resolution of symptoms. In order to quickly recognize this pathology, physicians need to be aware of it and familiar with the management. Further research is needed on the topic as studies thus far have been limited. This paper also demonstrates a need for more facilities with capabilities to perform emergent hyperbaric oxygen therapy.
Literary Sources
- Blanc P, Boussuges A, Henriette K, Sainty J, Deleflie M. Iatrogenic cerebral air embolism: Importance of an early hyperbaric oxygenation. Intensive Care Med.2002;28(5):559-563. doi:10.1007/s00134-002-1255-0
- Fakkert RA, Karlas N, Schober P, et al. Early hyperbaric oxygen therapy is associated with favorable outcome in patients with iatrogenic cerebral arterial gas embolism: systematic review and individual patient data meta-analysis of observational studies. Crit Care. 2023;27(1):1-7. doi:10.1186/s13054-023-04563-x
- Khazei A, Harrison D, Abu-Laban R, A-L, Mitra A. Potential missed cerebral arterial gas embolism in patients with in-hospital ischaemic stroke. Diving Hyperb Med. 2007;37(2):58-64. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L47322209.
- McCarthy CJ, Behravesh S behravesh@gmail com, Naidu SG, Oklu R. Air embolism: Diagnosis, clinical management and outcomes. Diagnostics. 2017;7(1):1-10.doi:10.3390/diagnostics7010005
- Murphy BP, Harford FJ, Cramer FS. Cerebral air embolism resulting from invasive medical procedures. Treatment with hyberbaric oxygen. Ann Surg. 1985;201(2):242245. doi:10.1097/00000658-198502000-00019
- White EG, Hayes HA, Clark P, Cloran FJ. Subclinical to catastrophic: a range of outcomes in cerebral air embolism. Emerg Radiol. 2023;30(6):823-827.doi:10.1007/s10140-023-02181-2

