3rd Place Emage Winner: A Subtle Presentation of Purpura Fulminans
Kayla Dueland-Kuhn, MD
SUNY Upstate University Hospital
Syracuse, NY
The patient was a 2-year-old female who presented to the pediatric emergency department via emergency medical services (EMS) in December due to respiratory distress, a “blue appearance,” and altered mental status. On arrival in the emergency department (ED), the patient appeared lethargic and tachypneic with peri-oral and peripheral cyanosis and she was brought immediately to a room for evaluation and placed on a monitor with intravenous (IV) access established. Initial vitals included a heart rate of 160, blood pressure of 94/50 and respiratory rate of 31. There was difficulty obtaining a pulse oximetry reading and the patient was placed on 15L oxymask due to concern of hypoxemia with subsequent O2 readings in the low 90s. The rectal temperature was 38.4°C. Our initial concern was focused on cardiopulmonary pathology; however, the lungs were clear to auscultation and a chest x-ray did not show pneumonia or cardiomegaly. A more detailed physical examination after initial stabilization revealed bilateral tympanostomy tubes and serous drainage and debris in the left ear canal, which parents stated was chronic. A very mild rash was noted on the distal right upper extremity. Upon removal of her diaper, scattered purpura was visible. She also had palatal petechiae. Within hours, her rash rapidly progressed, and she eventually developed purpura fulminans.
This case highlights the importance of a complete skin examination in pediatric patients, including diaper removal, and how rapidly disseminated intravascular coagulation (DIC) and purpura fulminans can progress. She required bilateral below-knee-amputations (BKAs) on day 20 of admission and was eventually diagnosed with Mondini dysplasia, which was the cause of chronic otorrhea and likely the initial source of infection. Cerebral spinal fluid (CSF) and blood cultures grew Streptococcus pneumococcus. Although the initial rash was subtle, the prompt recognition by our team helped with the diagnosis and treatment, and the patient was otherwise a happy child and is doing well today.

Figure 1: Right upper extremity on presentation.
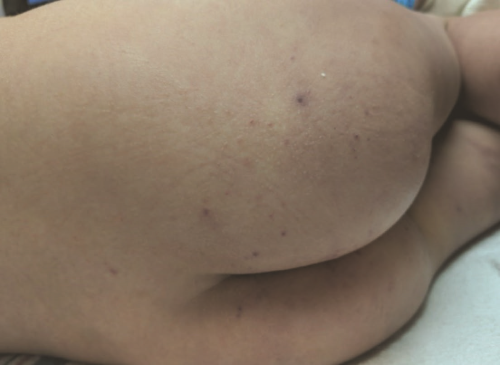
Figure 2: Gluteal rash on presentation.

Figure 3: Bilateral lower extremity rash 3 hours after initial presentation.

Figure 4: Right upper extremity, day 4 of admission.

Figure 5: Right lower extremity, day 4 of admission.

Figure 6: Bilateral lower extremities, day 18 of admission.