3rd Place Emage Winner: 3 AM Not Another Teenager Transferred for Persistent Vomiting: Not What You Expected
History of Present Illness
A 16-year-old healthy boy was transferred to the pediatric emergency department (PED) for 48 hours of vomiting. The patient had vomited a total of 40 times; emesis was yellow. There was no history of diarrhea, fever, or abdominal pain. Emesis was non-bloody. The patient denies fever, abdominal pain, constipation, and states passing gas today.
No history of migraines existed, and there were no headaches with this illness. The rest of the review of systems (ROS) was noncontributory.
The surgical and medical past medical history (PMH) was unremarkable.
At referral, intravenous (IV) resuscitation was initiated with labs and computed tomography (CT) scan was obtained.
The patient was referred for persistent vomiting and abnormal results.
Physical Examination
Blood pressure: 119/67 | Pulse: 92 | Temperature: 36.9 °C (Oral) | Respiration: 15 | SpO2 100%
Constitutional: Non-obese, slim, tall male, Glasgow Coma Scale (GCS) 15. He appeared well-developed, well-nourished, and under no distress.
HEENT (head, eyes, ears, nose and throat): Normal
Cardiovascular: Normal rate, regular rhythm, normal heart sounds, and intact distal pulses.
Pulmonary/Chest: Effort normal and breath sounds normal, No respiratory distress.
Abdominal: Soft, decreased bowel sounds (BS), mild distension of abdomen, mild guarding in all 4 quadrants
Musculoskeletal: Negative
Lymphadenopathy: Negative
Neuro: Normal
Labs
CBC (complete blood count) Basic |
Value | Value | |
| White blood cell (WBC) count | 13.47 | Lipase | 184 |
| Red blood cell (RBC) count | 4.58 | Comprehensive Metabolic Panel | |
| Hemoglobin | 13.9 | Glucose | 106 |
| Hematocrit | 38.9 | Blood urea nitrogen (BUN) | 25 (H) |
| Mean corpuscular volume (MCV) | 84.9 | Creatinine | 0.9 |
| Mean corpuscular hemoglobin (MCH) | 30.4 | Sodium | 137 |
| Mean corpuscular hemoglobin concentration (MCHC) | 35.8 | Potassium | 3.6 |
| Red cell distribution width (RDW) | 12.6 | Chloride | 105 |
| Platelets | 200 | CO2 | 20 (L) |
| Mean platelet volume | 8.2 | Calcium | 8.2 (L) |
| ABSOLUTE DIFFERENTIAL COUNTS | Total protein | 6.0 | |
| Neutrophils Absolute | 11.68 (H) | Albumin | 3.3 (L) |
| PERCENT DIFFERENTIAL COUNTS | Alkaline Phos | 110 | |
| Seg Neutrophils % | 86.7 (H) | Aspartate aminotransferase (AST) aka serum glutamic-oxaloacetic transaminase (SGOT) | 16 (L) |
| Lymphocytes % | 5.6 (L) | Alanine aminotransferase (ALT) aka serum glutamic-pyruvic transaminase (SGPT) | 13 |
| Monocytes % | 6.7 (H) | Bilirubin (Total) | 1.1 (H) |
| Eosinophils % | 0.8 | Anion gap | 15.6 |
| Basophil % | 0.2* | Amylase | 46 |
H-High value, L-Low value
Initial Chest X-ray
Findings: There is extensive pneumomediastinum with air dissecting along the esophagus, mediastinum, and supraclavicular soft tissues, along the lateral chest wall bilaterally, greater on the right.
No definite pneumothorax is visualized.

There is no focal consolidation. There is no pleural effusion. The heart size is normal. The bones are unremarkable.
Impression: Marked pneumomediastinum with air dissecting across the soft tissue planes.
Anterior-Posterior (AP) and Lateral Chest X-ray

Differential Diagnosis
Teenager with acute onset emesis and pneumomediastinum
- Cannabis hyperemesis syndrome
- Cyclic vomiting syndrome
- Ingestion - Mushrooms or illicit online medication
- Small bowel obstruction (SBO)
- Gastric outlet syndrome
- Central nervous system (CNS) causes tumor; idiopathic intracranial hypertension
- Bad case of acute gastroenteritis (AGE) or food poisoning
***The differential expanded even further after reviewing the outside CT scan with radiology.
Computed tomography downloaded from Occupational Safety and Health


CT Scan

YouTube link for the initial CT scan is available at https://youtu.be/jG0J2b3EhhU.
Impression
Extensive air surrounded the esophagus and within the mediastinum, with dissecting along soft tissue planes, as described, suggestive of an esophageal perforation.
There is no free air in the abdomen. There is dilated stomach and proximal duodenum, with narrowing of the duodenum as it crosses the superior mesenteric artery (SMA). This can be seen with SMA syndrome in the proper clinical setting.
ED Course
- Kept nothing by mouth (NPO) with maintenance of intravenous fluids (MIVF)
- Surgery strongly requested a nasogastric (NG) tube to be placed after reviewing CT despite concerns for esophageal perforation
- NG tube placed but on confirmatory CXR, the NG tube was noted to have drifted into left chest
- Surgery was immediately contacted, and the patient was prepped for the operating room to have the NG replaced under fluoroscopy.
Abdominal computed tomography angiography during hospitalization
FINDINGS (abbreviated): Normal robust enhancement of abdominal aorta, origins of celiac, superior mesenteric and renal arteries are demonstrated. The aortomesenteric angle measures 14 degrees. The aortomesenteric distance at the level of the duodenal crossing is 6 mm.


IMPRESSION:
- Interval resolution of previously demonstrated marked distention of the stomach. Proximal duodenum is mildly dilated, but significantly improved compared to prior.
- Both the aortomesenteric angle and aortomesenteric distance are decreased, as may be seen with SMA syndrome. Clinical correlation and follow-up care are recommended.
- Left chest tube is present with small left pneumothorax.
- Subcutaneous air is present with soft tissues in the lower chest.
- Small amount of posterior pneumomediastinum is present.
- Mild splenomegaly is present. The spleen appears elongated and relatively thin transversely.
Discussion: SMA syndrome
- Third portion of the duodenum passes between the aorta and the SMA
- Narrowing of the space between the superior mesenteric artery and aorta → compression of duodenum (and often left renal vein) → SBO
- Primarily attributed to loss of the intervening mesenteric fat pad

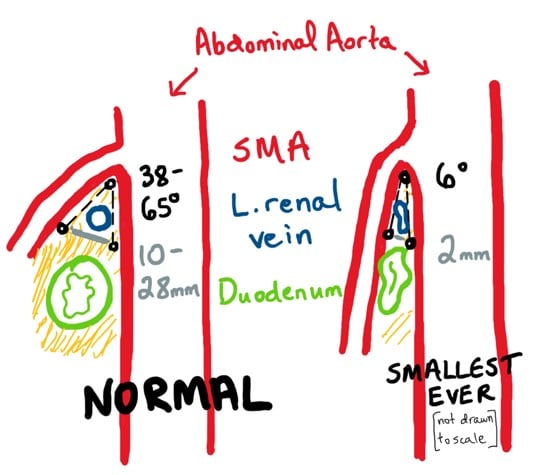

Drawings courtesy of Allison Auchter, MD, PhD
Discussion: Risk Factors
- Significant weight loss
- Anorexia nervosa, malignancy, malabsorption syndromes, AIDS, trauma, burns
- Anatomic abnormalities
- Congenital: short ligament of Treitz
- Acquired
- Surgery in pediatric population, most commonly after corrective surgery for scoliosis (“cast syndrome”)
- Celiac axis/compression syndrome
In the pediatric population, SMA syndrome can occur in otherwise healthy adolescents (usually after insufficient weight gain relative to height growth). The article by Biank et al (Biank V, Werlin S. Superior mesenteric artery syndrome in children: a 20-year experience. J Pediatr Gastroenterol Nutr. 2006 May;42(5):522-5. doi: 10.1097/01.mpg.0000221888.36501.f2. PMID: 16707974) shows no weight loss was found in 50% of the patients.
Discussion: Clinical Presentation
- Non-specific
- Mild: postprandial epigastric pain, early satiety
- Severe: intractable nausea, bilious emesis, weight loss
Physical Examination
- Non-specific
- Abdominal distension, succussion splash, and high-pitched bowel sounds
**The patient may get relief by lying prone in the left lateral decubitus or in a knee-chest position.
Labs
- Normal or significant electrolyte abnormalities
Discussion: Imaging
- Abdominal radiographs
- Upper GI series with oral contrast
- Conventionally: arteriography with barium contrast to demonstrate SMA superimposed upon the barium-filled duodenum
- CT and magnetic resonance (MR) arteriography have largely replaced conventional arteriography
- With ultrasound, it is possible to measure the aortomesenteric angle.
Discussion: Diagnosis
- Duodenal obstruction with an abrupt cutoff in 3rd portion.
- Aortomesenteric artery angle of ≤25° (most sensitive), particularly if the aortomesenteric distance is ≤8 mm. High fixation of the duodenum by the ligament of Treitz, low origin, or anomalies of the SMA
Discussion: Treatment
Conservative (preferred)
- NG tube, decompression (Concerns: NG placement if pneumomediastinum is present for esophageal perforation, which happened in this patient)
- Replete electrolytes
- Nutritional support until able to tolerate by mouth (PO)
- Enteral via nasojejunal (NJ) tube placed distal to obstruction
- Parenteral, if needed
- Gain weight
Surgical (if chronic or persistent)
- Strong’s procedure - divide ligament of Treitz
- Gastrojejunostomy
- Duodeno- jejunostomy
Hospital Course
The etiology was concerning for SMA syndrome. The patient was admitted to the Surgery Service post-operatively and kept NPO with NGT in place and total parenteral nutrition (TPN) started for nutrition. An upper gastrointestinal series (UGI)/esophagram was completed after one week of bowel rest showed no esophageal extravasation or duodenal obstruction. His bowel function returned, and he tolerated slowly advancing his diet. His CXR improved and CT was removed. A CTA completed confirmed the diagnosis of SMA syndrome (14-degree angle between aorta and SMA and 6 mm distance between vessel and duodenum). Non-surgical management of SMA syndrome was recommended given this was the first episode that the patient experienced, and surgery has variable results. Nutrition was consulted for a weight gain diet. By the day of discharge, the patient was tolerating a regular diet, afebrile >24 hours, and pain was controlled. The patient was discharged home in good condition with ~5lb weight gain.
Allison Auchter, MD, PhD
Medical College of Georgia
Mona Shah Kulkarni, MD and Thomas Abramo, MD
Children's Healthcare of Atlanta