
Stanford Emergency Critical Care Program (ECCP)
Background
The emergency department (ED) is equipped to provide initial diagnostic and resuscitative interventions for a broad range of critically ill patients 24/7. Unlike the intensive care unit (ICU), however, the ED is not designed to provide critical care for many hours or days. Nonetheless, when there is no available ICU bed, the ED is left with the task of providing close monitoring and frequent interventions over an extended period. Especially when multiple active ICU patients are boarding in the ED during the busiest hours of the day, sustaining high-quality critical care becomes difficult, as it interferes with the ability of ED providers to care for other patients. Even if the ICU team is officially responsible for the care of boarding patients, their ability to stay at the bedside is also limited by their need to care for other critically ill patients located elsewhere in the hospital. When neither the ED physician nor the admitting physician can devote sufficient time and attention to these vulnerable patients, it compromises the quality of care. Suboptimal care, especially during the golden hours of critical illness, may have a significant negative impact on the patients’ outcomes. The Stanford ECCP was created in August 2017 to address this very challenge; as dual-boarded emergency intensivists, we provide dedicated specialty care to critically ill patients in the ED, regardless of the ICU bed availability.
Targeted Patients for the ECCP
The following groups of patients were identified as the main populations likely to benefit from the ECCP:
- Patients boarding in ED due to lack of ICU beds.
- Undifferentiated patients: ED patients in need of critical care but without a clear initial ICU designation (ie, MICU vs. SICU vs. CCU vs. CVICU).
- Patients with borderline stability whom both the ward team and ICU team are reluctant to admit.
- Patients currently requiring ICU level of care, but with a high likelihood of stabilizing after a few hours of intense treatment in ED (ie, diabetic ketoacidosis (DKA)).
- Critically ill patients whose goals of care may not be aligned with ICU admission.
Program Description
Hours of Operation
The ECCP hours of operation are from 2:00 pm to midnight, Monday through Friday, including holidays. These hours were determined based on the average ED volume as well as patterns of arrival of critically ill patients to the ED.
Providers
All ECC physicians are dual emergency medicine (EM) and critical care medicine (CCM) board certified. Currently, we have three full-time and two per diem faculty in the program. We are also fortunate to have ECC RNs as part of our interdisciplinary program. These dual ED/ICU specialized nurses are staffed 24/7 and are primarily responsible for overseeing the care of critically ill patients in the ED. As partners, ECC physicians and ECC nurses work very closely to provide exceptional care for our patients.
Responsibilities
During ECC shifts, ECC physicians work as intensivists but spend the majority of our time in the ED to provide immediate evaluation and dedicated care for critically ill patients upon the requests of ED attendings. In the evening, we also see all newly admitted patients to the MICU, even if they are not admitted from the ED (ie, patients transferred to the MICU from the wards or other hospitals). We supervise MICU procedures and are available to help with any emergencies in the ICUs. Providing support and education for the trainees in the ED and MICU is another important responsibility.
Logistics in the ED
Terminology
- Level 1 patients: ED patients clearly requiring admission to ICU independent of initial management.
- Level 2 patients: ED patients currently requiring ICU level of care but likely to be downgraded to ward status within 6 hours (ie, asthma exacerbation, DKA, severe hyperkalemia).
- Consult-only patients: ED patients for whom intensivist consultation is requested but the ECC physician determines ICU-level care is not required.
Workflow
Critically ill patients are always evaluated and resuscitated by the primary ED team first. The ED attending decides if or when the ECC physician should be consulted for their patients. This preserves the autonomy and experience of the initial resuscitation for the ED team, which is a source of satisfaction and motivation for many emergency physicians (EP). The ED attending decides how long they want to keep their patients, based on their preference as well as the competing need of other patients in the ED. Upon request for consultation, the ECC physician immediately evaluates the patient and decides to which category the patient belongs (level 1, level 2, or consult-only). For level 1 MICU patients with readily available ICU beds, the ECC physician ensures a smooth transition of patient care from the ED to ICU. For level 1 MICU patients without ICU bed availability, level 1 undifferentiated patients, and all level 2 patients, an admission to the ECC service takes place without the need to move to a different bed. The ECC physician places all orders and promptly documents thought process, interventions, and relevant events as part of the ECC H&P. The care of Level 1 patients and level 2 patients who cannot be downgraded to ward status is transferred to the MICU team at the time of ICU bed availability or midnight, whichever comes first. The remaining level 2 patients are handed off to a ward team when the patient is downgraded. Of note, as soon as level 2 patients clinically declare the need for ICU admission or stability for downgrade, appropriate beds are requested, regardless of the time left before the 6-hour mark. For consult-only patients, the assessment and recommendations are communicated promptly to the ED team both verbally and in an ECC consultation note to facilitate timely dispositions (Figure 1).
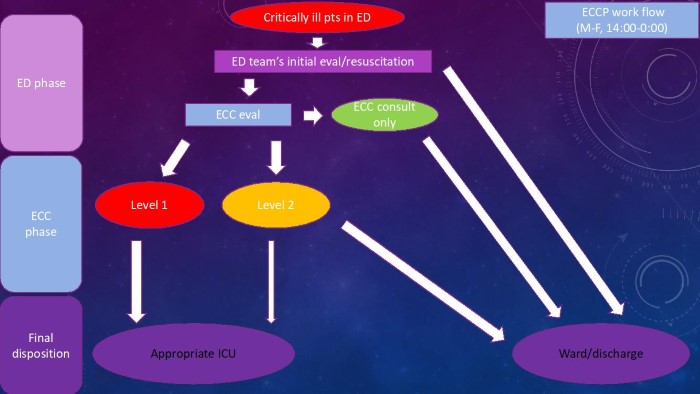
Figure 1. Stanford ECCP workflow
Six Areas of ECCP Benefit
Quality of care, education, research, throughput, resource allocation, and cost performance.
Higher Quality of Care/Improved Safety
Immediate and thorough evaluation by the ECC attending results in timely execution of key diagnostic testing, resuscitation, life-saving interventions, and compliance with key quality measures. It eliminates any care gap between the ED and ICU.
The dedicated role of the ECC physician allows frequent re-evaluations, early recognition of subtle changes, and timely interventions for any emergency/decompensation. We also accompany unstable patients during transport to ensure patient safety. By being able to closely monitor critically ill patients over time, we can better evaluate the trajectory of the patient and improve the safety and timing of the downgrading process. Additionally, the novel role allows us to promptly address both the physical and emotional needs of the critically ill patient and their family.
The ECC physician acts as the center of communication. Having the expertise and deep understanding of the unique challenges of both ED and ICU practice makes the ECC physician ideally suited for this role. We communicate closely with the patients, family, ICU team, ED team, consultants, ward team, bedside ED nurses, and ECC nurses to improve the care quality and safety. Of note, the on-call MICU attending is also kept abreast of all patients to ensure their inclusion into the care plan. Thorough and timely ECC documentation also helps other providers understand the details of the patient’s ED and ECC course.
Facilitation of early goals of care discussions for critically ill patients in the ED is crucial in setting the right path for the hospital course (or discharge to home hospice in some situations). For many reasons, however, arranging and conducting such discussions can be challenging for ED physicians during a busy shift. Patients may not have the capacity to make decisions, and surrogate decision makers may not be readily available. Some discussions may require input from primary care physicians, oncologists, palliative care specialists, or family from out of state. ECC faculty have the time and expertise to orchestrate such complicated, nuanced discussions.
Improved Education
EM residents: ECC faculty enhance critical care education for EM residents through bedside teaching and focused critical care group teaching. ECC faculty provide direct feedback on the initial resuscitation and continue to share the teaching points to the EM team throughout the ECC phase. If there is a pending procedure at the time of admission to the ECC service, we supervise EM residents. An ECC elective is also available for EM residents where they get individualized and dedicated critical care teaching at the bedside. When there are no critically ill patients in the ED, ECC faculty may take them to ICUs to teach variety of topics, such as mechanical ventilation, sedation, and vasopressors. Outside of the clinical setting, ECC faculty are also committed to the critical care education of EM residents through well-received EM-CCM joint conference series and simulation-based small group sessions called Critical Care Education Day.
ICU residents/fellows: The ECC faculty notify the ICU residents and fellows shortly after completing our preliminary assessment, so that they can get involved in the early stage of the resuscitation and maximize their learning. We pay attention to their level of training and preference, so that we can achieve the right balance of autonomy and supervision. Evening ICU house staff get direct teaching on their new admissions and supervision for all procedures by the ECC attending. When they need help with established ICU patients, we are also available to assist.
Enhanced Research Opportunities
The ECCP facilitates research focused on critically ill patients in the ED and on patients in ED ED-ICU interface. Not only are we studying the effect of our program on various outcomes, our presence also facilitates screening and protocol implementation for clinical trials that require enrollment of critically ill patients early in their disease course.
Improved Throughput
The ECCP contributes to improved throughput in multiple ways. First, we directly improve the throughput by providing faster disposition. We indirectly improve the departmental throughput by taking over the care of level 1 undifferentiated patients, level 1 patients without an ICU bed, and all level 2 patients including the downstream handoffs to inpatient services as described above. As a result, the primary ED team can devote their time to care for other patients and improve the ED flow.
Improved Resource Allocation
We do keep level 2 patients in the ED, even if there is an available ICU bed, and this can delay bed assignment for such patients. However, thus far more than 90% of level 2 patients have been downgraded successfully, thereby avoiding ICU admission. Besides reducing costs, this preserves ICU resources for patients with greater need.
Desirable Cost Performance
Because our program is a staffing model, there was no additional cost to acquire a separate space, equipment, or ancillary staff. The cost of operation is simply the cost of the ECC faculty, and it is covered by the revenue we generate. Staffing ECC faculty only during peak hours helps optimize the cost performance.
Acknowledgement
I would like to thank our ECC nurses, Jason Nesbitt and Chris Cinkowski, as well as our former EM-CCM fellows, Dr. Sara Crager and Dr. Julian Villar, who successfully designed and conducted the pilot program in the winter of 2016. Stanford ECCP was built upon this pilot program, and I could not have created this program without their passion. I would also like to thank Dr. S.V. Mahadevan and Dr. Matt Strehlow for their leadership and mentorship throughout the planning and implementation phase. I would like to thank all the ED and ICU colleagues for their understanding of and support for this program, which were absolutely necessary in its startup. Last, but not least, I would like to thank my ECC faculty colleagues, Dr. Shawn Kaku, Dr. Chris Walker, Dr. Jenny Wilson, and Dr. Alfredo Urdaneta, as well as the rest of our ECC nursing partners, Jim Mobley, Jennifer Kraft, Della Lau, and Claire Thomas. Special thanks to Dr. Jenny Wilson for her assistance in editing this article. The success of our program would not have been possible without their dedication to excellence in patient care, superb communications skills, and commitment to critical care education and research.
Tsuyoshi Mitarai, MD, FACEP
- Clinical Associate Professor, Director of Emergency Critical Care Program
- Assistant Director of Adult Emergency Medicine (Critical Care)
- Department of Emergency Medicine, Stanford University School of Medicine



