
Tips and Tricks: US-Guided Subclavian Vein
Introduction
Central venous catheters play an important role in the care of critically ill patients. The subclavian vein (SCV) is a deep central vein that is an extension of the axillary vein as it courses beneath the clavicle starting at the lateral border of the first rib before joining the internal jugular vein (IJV) medially under the clavicle. SCV cannulation offers several advantages when compared to the alternative sites, including fewer infectious complications, fewer cases of symptomatic deep venous thrombosis, and increased patient comfort.1 Despite the advantages that SCV central line offers, landmark-guided cannulation of the SCV can be associated with many complications such as arterial puncture, hematoma, pneumothorax, hemothorax, catheter malposition, and nerve injury.2
Ultrasound guidance for SCV cannulation has been explored and determined to be safe, effective, and efficient in reducing mechanical complications of SCV cannulation.3,4 There are different approaches to ultrasound-guided SCV cannulation: infraclavicular and supraclavicular approaches, which can be done “in-plane” (long-axis) and “out-of-plane” (short-axis). The short-axis view of the SCV is obtained by positioning the ultrasound probe perpendicular to the course of the vein. However, this approach does not allow for optimal visualization of the needle tip. The long-axis view, on the other hand, allows the provider to perform this using an “in-plane” approach which results in complete visualization of the full length of the needle. A single-center, randomized crossover control trial of 57 emergency medicine resident and attending physicians found that the long-axis approach resulted in more first-time attempt successes, fewer needle redirections, and reduced complications when compared with the short-axis approach.4 Another prospective, randomized crossover study of emergency medicine residents found that the long-axis approach for SCV cannulation was more efficient with decreased time cannulation and fewer needle redirections compared to the short-axis approach.5 Furthermore, the long-axis approach was also associated with fewer posterior wall punctures.5
As the SCV courses under the clavicle, it has a short supraclavicular course before it merges with the internal jugular vein to form the brachiocephalic vein. The confluence of these two major veins provides a large venous space that is easy to access with the supraclavicular approach. Although the infraclavicular approach is more commonly taught and used, there has been some limited evidence to suggest that the ultrasound-guided supraclavicular in-plane approach to SCV cannulation may be more favorable than the infraclavicular approach. A recent prospective, randomized study in children found that the supraclavicular approach had a lower time to cannulation, fewer attempts, and fewer misplacements than the infraclavicular approach.7 Given the limited space in the supraclavicular fossa, a standard high frequency endocavitary probe has been suggested as an advantageous technique in performing supraclavicular approach of SCV cannulation.8 In this Tips and Tricks, we describe both the supraclavicular and infraclavicular in-plane approaches to SCV cannulation.
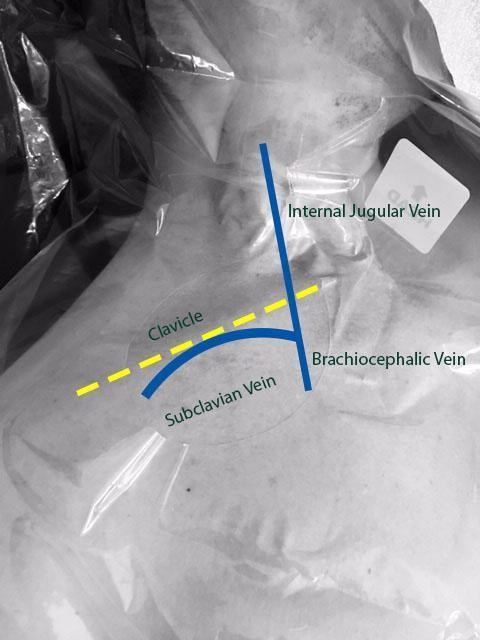
Figure 1. Anatomy of subclavian vein as it courses underneath the clavicle and merges with the internal jugular vein to form the brachiocephalic vein.
Technique:
A. Infraclavicular in-plane approach (Figure 2):
- Position the patient in the supine or Trendelenburg position. The patient should be prepped and draped in the usual sterile fashion. The ipsilateral IJV and the contralateral SCV areas should also be prepped and draped.
- Place a linear transducer (6-13 MHz) in the infraclavicular fossa, approximately 2-3 cm distal to where the SCV courses below the clavicle.
- Obtain a long-axis view of the axillary vein and the distal SCV. Evaluate the depth, caliber, and patency of the axillary vein and the SCV.
- Use compressibility and/or pulse-wave Doppler to confirm that the structure visualized is indeed the vein, and not the artery.
- Insert the needle in the midpoint of the small footprint transducer using the in-plane approach. The needle should be advanced slowly, taking note of the lung pleura underneath the vessels.
- If needle visualization is lost, it is important to stop advancing the needle. Withdraw slightly and re-visualize the needle before proceeding.
- Once within the lumen of the vessel, insert the guidewire and monitor the guidewire placement in real time with ultrasound.
- Make a small incision on the skin, dilate the vessel, and insert the catheter over the guidewire.

Figure 2: Ultrasound-guided subclavian vein cannulation. AXV (axillary vein), SCA (subclavian artery), SCV (subclavian vein).
B. Supraclavicular in-plane approach (Figure 3):
- Position the patient in the Trendelenburg position to allow venous engorgement and minimize the risk of air embolism. The patient should be prepped and draped in the usual sterile fashion. The ipsilateral IJV should also be prepped and draped.
- Place the transducer in the supraclavicular fossa abutting the ipsilateral clavicle. Angle the probe anteriorly to visualize the supraclavicular SCV. Slide the probe medially along the linear course of SCV until it’s confluence with the IJV is visualized.
- Evaluate the depth, caliber, and patency of the SCV and IJV. Use compressibility and/or pulse-wave Doppler to confirm that the structure visualized is indeed the vein, and not the artery.
- Insert the needle in the in-plane approach. The needle should be advanced slowly under direct visualization. The lung pleura lies underneath the vessel and must be approached with caution.
- If needle visualization is lost, it is important to stop advancing the needle. Withdraw slightly and re-visualize the needle before proceeding.
- Once within the lumen of the vessel, insert the guidewire and monitor the guidewire placement in real time with ultrasound. The guidewire location in right atrium/ventricle can also be rapidly confirmed by a subxiphoid view of the heart.
- Make a small incision on the skin, dilate the vessel, and insert the catheter over the guidewire.

Figure 3: Ultrasound-guided subclavian vein cannulation. EJV (External Jugular Vein), SCV (subclavian vein), SCA (subclavian artery).
In conclusion, the ultrasound-guided infraclavicular and supraclavicular approaches to SCV cannulation are safe and effective ways to decrease mechanical complications associated with SCV cannulation. Novice users must practice cannulation of other veins prior to SCV cannulation, as this technique is slightly more challenging.
References
- Parienti JJ, Mongardon N, Mégarbane B, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015;373(13):1220-9.
- Sterner S, Plummer DW, Clinton J, et al. A comparison of the supraclavicular approach and the infraclavicular approach for subclavian vein catheterization. Ann Emerg Med. 1986;15:421-4.
- Brass P, Hellmich M, Kolodziej L, et al. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015;1:CD011447.
- Fragou M, Gravvanis A, Dimitriou V, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39(7):1607-12.
- Sommerkamp SK, Romaniuk VM, Witting MD, et al. A comparison of longitudinal and transverse approaches to ultrasound-guided axillary vein cannulation. Am J Emerg Med. 2013;31(3):478-81.
- Vogel JA, Haukoos JS, Erickson CL, et al. Is long-axis view superior to short-axis view in ultrasound-guided central venous catheterization? Crit Care Med. 2015;43(4):832-9.
- Byon HJ, Lee GW, Lee JH, et al. Comparison between ultrasound-guided supraclavicular and infraclavicular approaches for subclavian venous catheterization in children--a randomized trial. Brit J Anaesthes. 2013;111(5):788-92.
- Mallin M, Louis H, Madsen T. A novel technique for ultrasound-guided supraclavicular subclavian cannulation. Am J Emerg Med. 2010;28(8):966-69
Yanika Wolfe, MD; Vidit Bhargava, MBBS
Viveta Lobo, MD, FACEP
Stanford University

