Ultrasound Guided Suprapatellar Recess Injection for Knee Pain in the Emergency Department
Katherine Vlasica, DO FACEP
St Joseph's Health, Paterson, NJ
Christine Collins, MD
Cooper University Hospital, NJ
Knee pain is a common presentation in the emergency department (ED), often requiring prompt pain management to alleviate discomfort and facilitate disposition. A suprapatellar recess injection, guided by ultrasound, is a valuable procedure that emergency physicians can employ to provide targeted relief.
Two commonly considered options for targeted pain management are the suprapatellar recess injection and the genicular nerve block. While both techniques aim to alleviate knee pain, several advantages make the suprapatellar recess injection a favorable choice in the ED setting.
Precision of Targeting
One of the primary advantages of suprapatellar recess injection is their ability to directly target the intra-articular space of the knee joint. By accessing the suprapatellar recess, located above the patella and within the joint capsule (Figure A), clinicians can deliver medications such as corticosteroids or local anesthetics precisely. This targeted approach ensures that therapeutic agents reach the site of inflammation or injury directly, enhancing efficacy and minimizing systemic side effects.
In contrast, genicular nerve blocks involve targeting the nerves surrounding the knee joint. While effective in providing pain relief by interrupting nociceptive pathways, a genicular block may not address intra-articular pathology. This distinction is crucial, especially in cases where inflammation or synovial irritation within the joint space is the primary source of pain. In addition, the genicular block involves multiple injections over the fibula and the femur, which can be painful, making it less ideal for the ED setting.
Indications
- Knee pain secondary to inflammatory conditions such as osteoarthritis, rheumatoid arthritis, or synovitis.
- Acute exacerbations of chronic knee pain.
- Diagnostic purposes to confirm intra-articular pathology when other modalities are inconclusive.
Contraindications
- Septic arthritis or suspected joint infection.
- Skin infection at the injection site.
- Coagulopathy or bleeding disorders that increase the risk of hematoma formation.
- Allergy to any components of the injected medication.
Procedure
- Informed Consent: Obtain informed consent after explaining the procedure, potential risks, and benefits.
- Patient Positioning: Position the patient comfortably with the knee slightly flexed to relax the quadriceps muscles.
- Prescan: Place the ultrasound probe in a short-axis position above the patella. Identify the femur and locate the first tissue layer above it, which is the suprapatellar fat pad. The suprapatellar recess appears as an anechoic pocket above the suprapatellar fat pad and posterior to the quadriceps tendon. Note the depth of the recess in relation to the probe; this will guide the needle insertion, which should be parallel to the floor.
- Cleaning: Strict aseptic technique is essential as you are entering the joint space. Clean the skin at the injection site using chlorhexidine or iodine. Use sterile gloves throughout the procedure.
- Ultrasound Setup: Apply a sterile ultrasound probe cover and ultrasound gel to the probe. Place the probe in a short-axis position above the patella and identify the suprapatellar recess again for accurate needle placement.
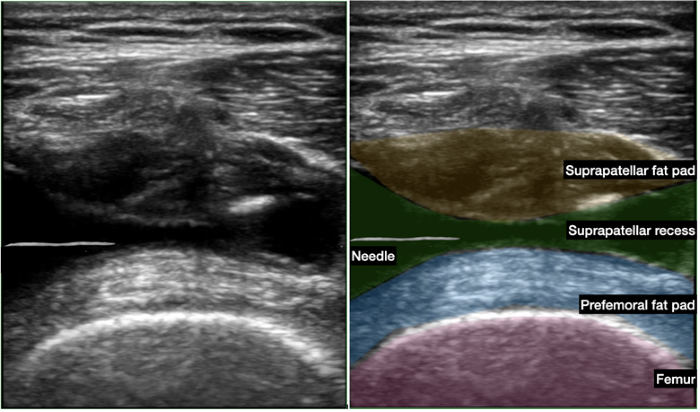
- Needle Insertion: Choose an appropriate needle length (typically 1.5 to 2 inches) and gauge (eg, 21- or 22-gauge) for the injection. Insert the needle parallel to the probe in a lateral to medial direction at the depth of the suprapatellar recess identified during the prescan (Figure B). Use ultrasound guidance while visualizing the needle tip to confirm the needle's entry into the suprapatellar recess.
- Medication Administration: Administer the prescribed medication (eg, Triamcinolone is standard) mixed with 4-5 ml of local anesthetic. Ensure slow and steady administration while monitoring under ultrasound for accurate placement and to avoid vascular uptake (Figure C).
Conclusion
An ultrasound guided suprapatellar recess injection is a safe and effective procedure for managing knee pain in the ED setting. It allows for precise localization of medication delivery, thereby optimizing therapeutic outcomes while minimizing risks. Emergency physicians trained in ultrasound-guided techniques can confidently perform this procedure, offering timely relief to patients presenting with acute or chronic knee pain. Strict adherence to cleaning protocols, careful patient selection based on indications, and awareness of contraindications are crucial to ensuring the success and safety of this intervention.
In conclusion, integrating suprapatellar recess injections into the repertoire of emergency procedures enhances the comprehensive care provided to patients with knee pain, reinforcing the ED's role in managing musculoskeletal emergencies effectively.
Resources
Chagas-Neto FA, Taneja AK, Gregio-Junior E, Nogueira-Barbosa MH. In-Plane Ultrasound-Guided Knee Injection Through a Lateral Suprapatellar Approach: A Safe Technique. Ultrasound Q. 2017;33:139-143.
Maricar N, Parkes MJ, Callaghan MJ, Felson DT, O'Neill TW. Where and how to inject the knee--a systematic review [published correction appears in Semin Arthritis Rheum. 2015;44(5):e18] [published correction appears in Semin Arthritis Rheum. 2015 Apr;44(5):e18.
Wu WT, Chang KV, Naňka O, Mezian K, Ricci V, Wang B, Özçakar L. Ultrasound Imaging of the Articularis Genus Muscle: Implicatons for Ultrasound-Guided Suprapatellar Recess Injection. Diagnostics (Basel). 2024;14(2):183.
Figure A. Graphic depicting the suprapatellar recess (star)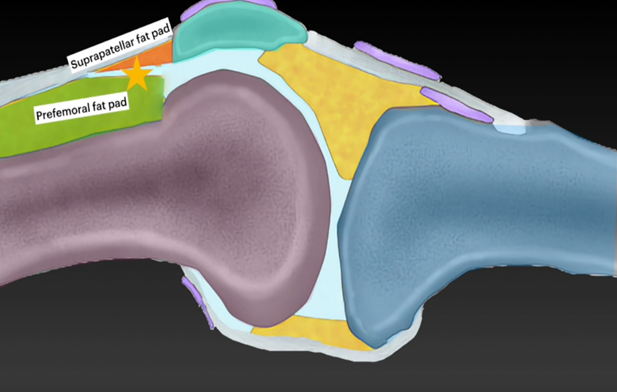
Figure B. Anatomical positioning of ultrasound as well as recommended needle positioning (parallel to probe)
Figure C. Ultrasound images of injection depicting injection into the suprapatellar recess. Needle is in between the suprapatellar fat pad (yellow) and prefemoral fat pad (blue)