
TEE and Area of Maximal Compression
Robert Stenberg, MD, FACEP
Cleveland Clinic Akron General
Natalie Truong, MD
Loma Linda
Charge nurse announces, “Cardiac arrest, 5 minutes out.” Team assembles. The patient is a male in his 60’s with multiple comorbidities that had a witnessed arrest in front of spouse. Paramedics placed humeral intraosseous access and a supraglottic airway. Total downtime 15 minutes in pulseless electrical activity (PEA) arrest throughout, with three rounds of epinephrine.
Upon arrival, an automated chest compression device was in place with ongoing cardiopulmonary resuscitation (CPR), end-tidal CO2 20mmHg, and had just received epinephrine. Patient moved to the gurney and is pulseless; CPR resumed. Supraglottic airway is immediately removed for a definitive endotracheal tube, while compressions were ongoing. Transesophageal echocardiography (TEE) transducer inserted after appropriate considerations were taken, and this is seen.
Figure 1. Shows ongoing chest compressions in the midesophageal long axis view (MeLAX). With the compressions it is noted the area of maximal compression (AMC) is over the left ventricular outflow tract (LVOT) and aortic valve (AV).
Based on TEE, the AMC is adjusted by moving the chest compression location inferolaterally. TEE remains in place and shows this after adjustment.
Figure 2. Shows ongoing chest compressions in the MeLAX, which after adjustment is now over the LV
End-tidal noticed to rise. Two minutes later, repeat pulse check demonstrates return of spontaneous circulation (ROSC). Further resuscitative efforts were made and the patient was successfully transferred to the intensive care unit with eventual neurologically intact and discharge.
This case highlights the use of resuscitative TEE in cardiac arrest to optimize AMC and improve ROSC. Resuscitative TEE has a multitude of benefits in the setting of shock and arrest with a growing body of literature; further, it is an attainable skill for Emergency Physicians with appropriate training (please refer to updated June 2023 ACEP TEE Guidelines here: https://www.acep.org/patient-care/policy-statements/use-of-transesophageal-echocardiography-tee-in-the-ed-for-shock-cardiac-arrest-and-procedural-guidance).1-7
One of the most rapidly growing bodies of literature on resuscitative TEE focuses around the AMC and obtaining ROSC. Most recently, published in Critical Care Medicine May 2024, a single center in Taiwan performed a prospective observational cohort.7 It was discovered of the 76 enrolled, 37 had evidence of AV compression on TEE and those that did not have compression noted had more favorable outcomes:
|
Outcome |
Compressed AV |
Uncompressed AV |
Adjusted Odds Ratio |
P value |
|
Sustained ROSC |
24.3% |
53.8% |
4.72 |
0.010 |
|
Any ROSC |
32.4% |
56.4% |
3.30 |
0.033 |
|
Survival to ICU |
8.1% |
33.3% |
6.74 |
0.010 |
|
Initial diastolic blood pressure |
11.5mmHg |
33.4mmHg |
- |
0.002 |
|
Achieve diastolic pressure above 20mmHg during CPR |
93.8% |
33.3% |
|
<0.001 |
Figure 3. Table of recent prospective paper highlighting difference in outcomes regarding AMC
A simplified concept of this, is if one is squishing a water balloon and squishing the outlet of the balloon at the same time, there will be minimal to no forward flow. To assess this, it is often best to obtain a MeLAX view. Once the probe is inserted, a MidEsophageal 4 Chamber view (Me4Ch) can easily be identified. From there, the omniplane is rotated to approximately 120 degrees, until the left ventricular inflow and outflow are well visualized. Then it is assessed whether the AMC is over the AV or more appropriately over the LV. If the AMC is felt to be compressing the LVOT/AV, the location of chest compressions should be adjusted inferolaterally.
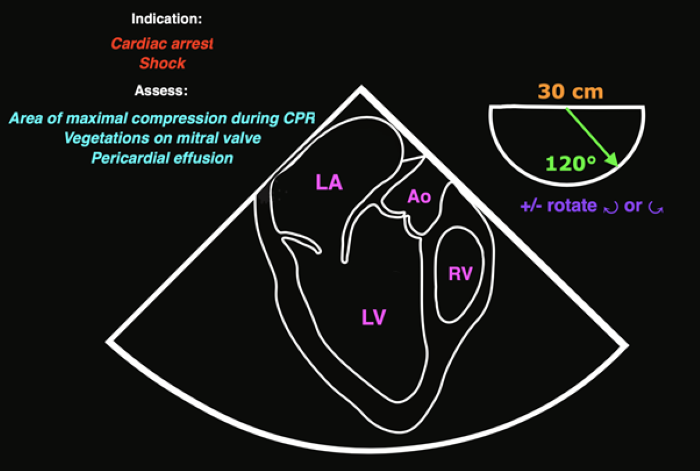 Figure 4. TEE Card showing MeLAX
Figure 4. TEE Card showing MeLAX
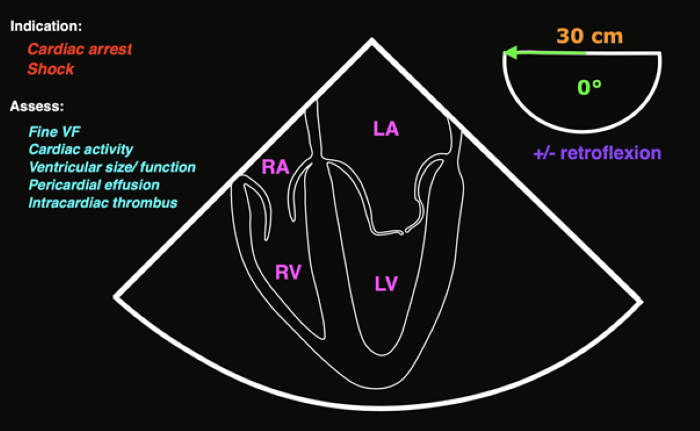 Figure 5. TEE Card showing Me4Ch
Figure 5. TEE Card showing Me4Ch
Refer to Dr. Felipe Teran’s Resuscitative TEE Project website @ https://www.resuscitativetee.com/, and also refer to ACEP’s growing TEE Roadmap to help programs start up TEE: https://sites.google.com/view/tee-roadmap/home
References
- American College of Emergency Physicians. Use of Transesophageal Echocardiography (TEE) in the ED for Shock, Cardiac Arrest, and Procedural Guidance [policy statement] approved June 2023. https://www.acep.org/patient-care/policy-statements/use-of-transesophageal-echocardiography-tee-in-the-ed-for-shock-cardiac-arrest-and-procedural-guidance
- Resuscitative TEE Project. https://www.resuscitativetee.com/
- TEE Program Starter Kit. Accessed at: https://sites.google.com/d/12FoEcmIJ_pD9HiqbFTxEdzU65YTRZg9A/p/13Woh229DLDNpDQB80WSTHfy95cFsLbtz/edit
- Anderson KL, Fiala KC, Castaneda MG, Boudreau SM, Arana AA, Bebarta VS. Left ventricular compressions improve return of spontaneous circulation and hemodynamics in a swine model of traumatic cardiopulmonary arrest. J Trauma Acute Care Surg. 2018;85(2):303-310. Accessed at: https://pubmed.ncbi.nlm.nih.gov/29613954/
- Teran F, Dean AJ, Centeno C, Panebianco NL, Zeidan AJ, Chan W, Abella BS. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-147. Accessed at: https://pubmed.ncbi.nlm.nih.gov/30779977/
- Teran F, Sands N, Wray T, on behalf of the Resuscitative TEE Collaborative Registry Investigators. Abstract 200: Left-ventricular Outflow Compression During Cardiopulmonary Resuscitation Is Associated With Lower Return Of Spontaneous Circulation In Out-of-hospital Cardiac Arrest. 2022;146(Suppl 1). Accessed at: https://www.ahajournals.org/doi/10.1161/circ.146.suppl_1.200
- Chu S, Huang C, Cheng C, et al. Cardiopulmonary Resuscitation Without Aortic Valve Compression Increases the Chances of Return of Spontaneous Circulation in Out-of-Hospital Cardiac Arrest: A Prospective Observational Cohort Study. Crit Care Med. 2024;52(9): 1367-1379. Accessed at: https://pubmed.ncbi.nlm.nih.gov/38780398/

