
Riders on the Storm: Stellate Ganglion Block for Electrical Storm
Brian Makowski, DO
Joshua Jacquet, MD, FACEP
Trent T. She, MD, FACEP
Kevin Watkins, MD, FACEP
Robert T. Stenberg, MD, FACEP
Case Presentation
A 52 year-old-male presents via triage diaphoretic and clutching his chest. The patient states around 30 minutes ago he began to experience fluttering in his chest that subsequently turned into sharp midsternal chest pain. He reports a past medical history of hypertension and heart failure, however he often forgets to take his daily medications. His initial vital signs are as follows: T 97.8°F, HR 110bpm, BP 80/40 mmHg, RR 24, and SpO2 of 95% on room air. As you begin to examine him you notice rapid, thready pulses that quickly vanish. The patient becomes unresponsive, pulseless and ACLS is begun. At the first pulse check, the rhythm on the Zoll is displayed below in Figure 1. Defibrillation is delivered, and ACLS is resumed. Multiple rounds of ACLS are performed with each pulse check demonstrating the same rhythm as in Figure 1.
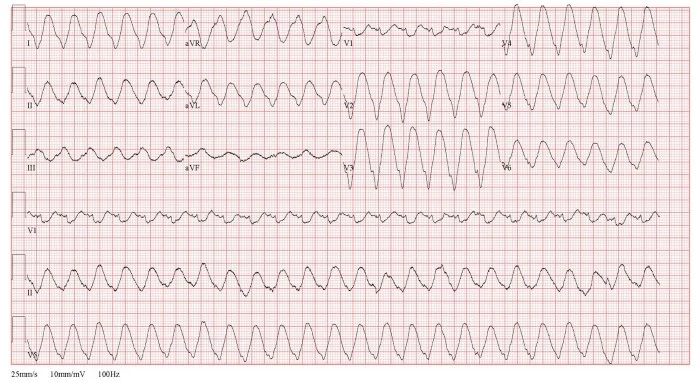 Figure 1. Monomorphic Ventricular Tachycardia. Used with permission, Brian Makowski, DO
Figure 1. Monomorphic Ventricular Tachycardia. Used with permission, Brian Makowski, DO
Background
Electrical storm (ES), sometimes called ventricular storm, is defined as the occurrence of three or more episodes of sustained ventricular tachycardia (VT) or ventricular fibrillation (VF) in a short period of time (often 24 hour window).1 While multiple underlying etiologies may be responsible for causing ES, it is additionally perpetuated by sympathetic activation which decreases the threshold for ventricular arrhythmias and refractoriness.
Traditional management includes Advanced Cardiac Life Support (ACLS)-guideline driven resuscitation if the patient is pulseless, with amiodarone as first line antiarrhythmic therapy, followed by beta-blockade with either propranolol, esmolol, or metoprolol. One caveat to following ACLS guidelines is that attempts should be made to minimize use of epinephrine as much as possible considering treatment of ES revolves around sympathetic blockade, and beta-blockade in these patients has shown to have a higher survival rate compared to ACLS antiarrhythmics (67% vs. 5%).2
Other considerations may include use of dual sequential defibrillation, changing pad location (especially switching from anterolateral to anteroposterior), aggressive electrolyte repletion (ie, magnesium, potassium, and calcium), veno-arterial extracorporeal membrane oxygenation (VA ECMO), and use of phenylephrine as a first line vasopressor as it is a pure alpha-1 adrenergic agonist and will not stimulate cardiac beta-receptors.3,4 Sometimes, these efforts are unsuccessful at terminating the arrhythmia.
The Stellate Ganglion Block (SGB) provides an adjunct in treatment when ES is refractory to traditional management. It is considered one type of cervical sympathetic block; and has not only been proven to be a safe and effective treatment modality in ES, but is also used for a multitude of indications, including PTSD, phantom limb pain, complex regional pain syndrome, zoster of head/neck/upper extremity, and other autonomic-related conditions.5-9 There is also growing evidence for use in the neurocritical care patient population to reduce vasospasm for conditions such as aneurysmal subarachnoid hemorrhage.10
For Emergency Medicine, the primary indication for SGB is to abort electrical/ventricular storm. The goal of the SGB in ES is to cause cardiac sympathetic denervation through blockade of the sympathetic chain at the inferior ganglion (also known as the stellate ganglion due to its star-shaped appearance). Blockade at this level targets sympathetic outflow to the myocardium, subsequently increasing the threshold for arrhythmia and allowing for further resuscitative efforts to be successful.
Key Recent Publications
- The STAR Study11
- Multi-Center (19 centers), International Retrospective & Prospective Longitudinal Study
- 131 patients, 184 total SGB’s performed
- 82% patients had bolus only
- 42% of procedures were ultrasound-guided
- Anesthetic used (% of cases)
- Lidocaine alone, 28%
- Bupivacaine alone, 4.3%
- Lidocaine + bupivacaine, 23.9%
- Lidocaine + ropivacaine, 34.2%
- Primary Outcomes = Efficacy & Safety
- 92% of patients showed a reduction of antitachycardia pacing or defibrillation shocks >50% in the 12 hours following SBG
- Only 1 major complication occurred (0.5%)
- One case of Local Anesthetic Systemic Toxicity (LAST), that had respiratory suppression and was successfully corrected with lipid emulsion therapy
- Secondary Outcomes
- Anisocoria
- Not all patients with a successful block will have anisocoria: 56% did not have anisocoria with no difference in reduction of dysrhythmia between groups.
- Anatomic versus ultrasound-guided, bolus vs infusion
- Significant reduction of treated arrhythmias in both anatomical and ultrasound-guided groups
- No significant difference between bolus and continuous infusion groups
- High volume versus Low Volume
- Similar efficacy in high volume and low volume centers
- Dual antiplatelet therapy and anticoagulation
- No complications with patients on antiplatelet therapy or anticoagulation (67% blocks)
- Mild complications
- Minor
- Bradycardia 1 case (0.5%)
- Hypotension 1 case (0.5%)
- Expected Side Effects of Block
- Temporary brachial plexus 3 cases (1.6%)
- Hoarseness 2 cases (1.1%)
- Dysphonia/Neck Pain/Vomiting 1 case each (0.5%)
- Savastano S, Baldi E, Compagnoni S, et al. Electrical storm treatment by percutaneous stellate ganglion block: the STAR study. Eur Heart J. 2024;45(10):823-833. doi:1093/eurheartj/ehae021
- Minor
- Meta-analysis published this fall:12
- 15 studies, 542 patients, 553 ES events
- Demonstrated a significant reduction in ventricular arrhythmia with SGB:
- 70% complete resolution of ventricular arrhythmia (VA)
- 19% had partial resolution of VA
- 7% had no resolution of VA
- Motazedian P, Quinn N, Wells GA, et al. Efficacy of stellate ganglion block in treatment of electrical storm: a systematic review and meta-analysis. Sci Rep. 2024;14:24719. https://doi.org/10.1038/s41598-024-76663-9
- New case series Nair, et al:13
- Two scenarios with resolution of ES by left SGB using 10mL 2% Lidocaine
- One after amiodarone bolus x2, lidocaine bolus, and esmolol bolus. Resolution of ventricular tachycardia within five minutes.
- One after amiodarone bolus and infusion with “pharmacologic cardioversion”; resolution of dysrhythmia after block
- Two scenarios with resolution of ES by left SGB using 10mL 2% Lidocaine
- Anisocoria
Procedure
Generally, the block should be performed on the left side, as there is more evidence for left-sided block; and, in some studies, there has been a decreased rate of hypotension with a left-sided block. In a review of 16,404 right SGB and 13,766 left SGB, the right SGB decreased blood pressure by 25-49mmHg in 10.9% of cases and more than 50mmHg in 0.67% with only 4% cases with increase in pressure; on the other hand, the left SGB decreased blood pressure by 25-49mmHg in 8.4% and more than 50mmHg in 0.49% with an increase in blood pressure in 6.2% of cases. Further, the right SGB had a 30 beats per minute drop in heart rate relative to left SGB.14, 15
To determine whether the block was successful, the primarily means of evaluating such should be reduction in VA. Prior thought of assessing for Horner’s syndrome (ptosis, miosis, anhidrosis) for block success was demonstrated to not be reliable in the STAR trial.11
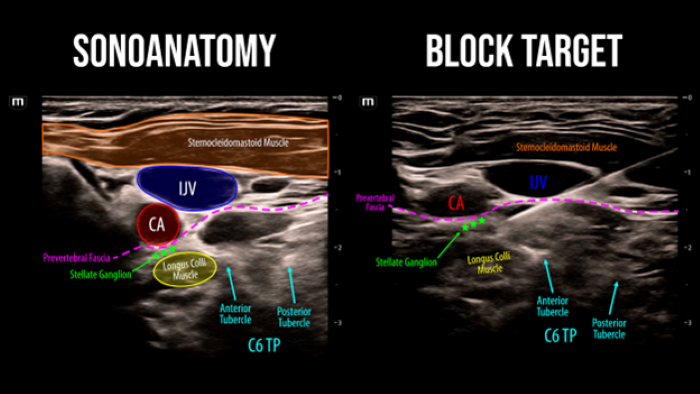 Figure 2. SGB Sonoanatomy and block target. Used with permission Brian Makowski, DO
Figure 2. SGB Sonoanatomy and block target. Used with permission Brian Makowski, DO
- Indications:
- Electrical Storm
- Contraindications:
- Anaphylaxis to local anesthetic
- Anticoagulation is NOT a contraindication (refer to STAR Study above); recommend providers use risk benefit and clinical decision-making
- Medication Selection:
- Although variable in literature, typically around 10 mL of a short-acting local anesthetic is used, such as 1% or 2% lidocaine withOUT epinephrine
- A longer acting anesthetic has the significant benefit of extending the duration of blockade; on the other token, any complications will have a longer duration.
- Some studies also used dexamethasone to further extend the action of blockade, typically 8mg; this should be preservative-free 16,17
- Set-up/positioning:
- Get medications and nerve block equipment
- Nerve block needle, micropuncture needle or blunt-tipped needle strongly preferred to reduce trauma to surrounding structures
- Consider placing the ultrasound machine to the right side of the patient near the head/neck while standing on patient’s left for optimal ergonomics
- Turn the patient's head contralaterally (to the right). This exposes the neck for easier needle entry and to have a clearer needle trajectory as it can displace internal jugular vein (IJ) and other vessels out of the way
- Get medications and nerve block equipment
- Procedure
- Place transducer, in a transverse orientation, along the left side of the neck around the level of the thyroid (C6), near where you would for an IJ central line (Figure 2)
- Some experts recommend tracking the brachial plexus nerve roots from the supraclavicular region cranially to track where the C6 nerve root originates as a means to ensure ultrasounding the appropriate level.18
- Identify the carotid artery, and make small sweeps cranially and caudally until you can see a defined muscle belly deep to the carotid (longus colli muscle) without any vital structures lateral to the area for safe needle approach.19
- Use color/power Doppler to ensure a safe needle trajectory, particularly watching for vessels such as inferior thyroid and vertebral artery
- Insert needle in-plane, lateral to medial, advancing needle towards the prevertebral fascia, along superficial aspect of the longus colli muscle just deep to carotid. Try to avoid nerve fascicles, vessels and the esophagus along the needle trajectory
- It can be hard at times to get around the anterior C6 tubercle (also known as Chassaignac’s tubercle), and some resources recommend trying to sweep just caudal to this area to access.
- Anchoring hands for transducer stability and needle control will be essential if performing during chest compressions
- Aspirate, then inject 10mL of anesthetic. (Figure 3)
- If no improvement, one can consider blocking the right stellate ganglion in similar fashion (a 10 minute window is often considered a fair time to wait in between).20
- Consider the total dose of local anesthetic the patient has received in attempts to avoid LAST Syndrome.
- If using lidocaine, may need to repeat bolus with the shorter duration of action
- Place transducer, in a transverse orientation, along the left side of the neck around the level of the thyroid (C6), near where you would for an IJ central line (Figure 2)
- Complications21
- Most common complications are transient
- Most common are hoarseness (up to 28%) and lightheadedness (up to 7.6%)
- Others include hypertension, cough, Horner's, brachial plexus block, and hematoma.
- Please review STAR trial complications above, highlighting a modern practice done with the indication of ES. There were minimal major complications and a few transient expected complications.11
- There are rare case reports of more serious outcomes, many of which were done without ultrasound guidance, and perhaps with outdated equipment (sharp needles, etcetera).
- There are rare case reports of seizure, cardiac arrest, pneumothorax, infection, dural puncture, hemomediastinum
- Most common complications are transient
Consider having resuscitative equipment nearby (which is very likely the case, already)
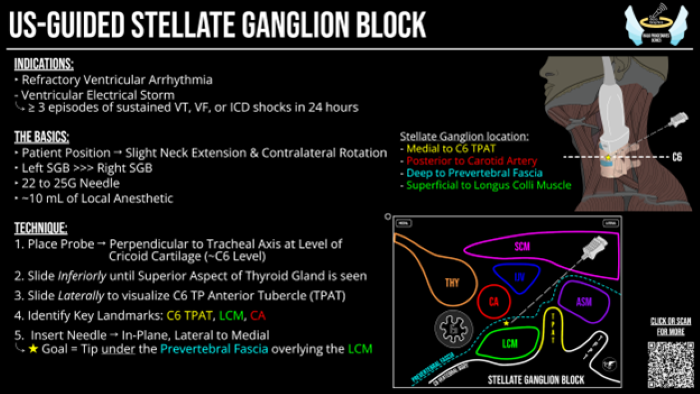 Figure 3. SGB HALO Procedure Pocket Card. Used with permission Brian Makowski, DO
Figure 3. SGB HALO Procedure Pocket Card. Used with permission Brian Makowski, DO
The Challenge: not whether, but when?
There is now a solid body of evidence showing SGB has good reduction in ventricular arrhythmia in the setting of ES. The challenging question is when in your algorithm does the SGB fit in?
To the best of the author’s knowledge there is no consistent evidence or guidelines regarding where this piece fits in the algorithm. The only information found was from 2017 AHA/ACC/HRS Guidelines on VT/VT, highlighting the following:
“In patients with VT/VF storm in whom a beta blocker, other antiarrhythmic medications, and catheter ablation are ineffective, not tolerated, or not possible, cardiac sympathetic denervation may be reasonable.” 22
Many have considered it when reaching for or administering esmolol.23 One other thought, with the case of LAST syndrome in the STAR trial, there may be some consideration of performing the block prior to multiple doses of intravenous lidocaine; based on this, one could consider performing block after one intravenous bolus of lidocaine, perhaps while administering beta blocker intravenous bolus. Lastly, there is some concern whether this block is being done at a point in the resuscitation at which a chance of recovery is minimal, and it may be worth performing at a point of the resuscitation while the patient has a more meaningful chance of recovery.
Case Resolution
The patient had two rounds of antiarrhythmic medications and pads were switched from anterolateral to anteroposterior; despite aggressive efforts, criteria was met for refractory ventricular tachycardia with Electrical Storm. 10mL of 1% lidocaine was applied to the stellate ganglion under ultrasound guidance during CPR and the dysrhythmia resolved, resulting in return of spontaneous circulation (ROSC). Post-ROSC ECG demonstrated an occlusion myocardial infarction resulting in a cardiac catheterization and successful drug eluting stent. The patient later walked out of the hospital neurologically intact.
Summary
There is now substantial evidence supporting SGB in managing ES, demonstrating its efficacy and safety profiles; it should be considered in refractory ES, and may be more impactful at a center that does not readily have access to VA ECMO. To the best of the authors’ knowledge, there is no evidence to demonstrate a mortality benefit. Hopefully, the randomized controlled study enrolling patients until December 2024, theGANGlion Stellate Block for Treatment of Electric storRm Trial (GANGSTER Trial) can further add to the evidence.24
While it is fair to perform a landmark-based approach, emergency physicians easily have the skillset to perform this under ultrasound guidance and there is evidence of decreased complications with such. A reasonable plan is a single injection of 10mL of 1% lidocaine along the left stellate ganglion; anisocoria is not a reliable marker for success and reduction in ventricular arrhythmia should be the primary focus for block success. A large challenge is navigating the timing upon which this is performed in the emergency department with other more standard measures. One can apply their clinical judgement based on the multitude of variables, or consider performing after having given two to three antiarrhythmic medications and making other adjustments.
References
- Eifling M, Razavi M, Massumi A. The evaluation and management of electrical storm. Tex Heart Inst J. 2011;38(2):111-21.
- Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm : sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation. 2000;102(7):742-747.
- Lupton JR, Newgard CD, Dennis D, et al. Initial Defibrillator Pad Position and Outcomes for Shockable Out-of-Hospital Cardiac Arrest. JAMA Netw Open. 2024;7(9):e2431673.
- Cheskes S, Verbeek PR, Drennan IR, McLeod SL, Turner L, Pinto R, et al. Defibrillation Strategies for Refractory Ventricular Fibrillation. N Engl J Med. 2022;387(21):1947-1956.
- Narouze S. Ultrasound-guided stellate ganglion block: safety and efficacy. Curr Pain Headache Rep. 2014;18(6):424.
- Carron H, Litwiller R. Stellate ganglion block. Anesth Analg.1975;54(5):567-70.
- Rae Olmsted KL, Bartoszek M, Mulvaney S, McLean B, Turabi A, Young R, et al. Effect of stellate ganglion block treatment on posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Psychiatry. 2020;77(2):130-38.
- Elias M. Cervical Sympathetic and Stellate Ganglion Blocks. Pain Physician. 2000;3(3):294-304.
- Feigin G, Figueroa SV, Englesakis MF, D’Souza R, Hoydonckx Y, Bhatia A Stellate ganglion block for non-pain indications: a scoping review. Pain Med. 2023;24(7):775-781.
- Bombardieri AM, Albers GW, Rodriguez S, Pileggi M, Steinberg GK, Heit JJ. Percutaneous cervical sympathetic block to treat cerebral vasospasm and delayed cerebral ischemia: a review of the evidence. J Neuronterv Surg. 2023;15(12):1212-1217.
- Savastano S, Baldi E, Compagnoni S, Rordorf E, Sanzo A, Gentile FR, et al. Electrical storm treatment by percutaneous stellate ganglion block: the STAR study. Eur Heart J. 2024;45(10):823-833.
- Motazedian P, Quinn N, Wells GA, et al. Efficacy of stellate ganglion block in treatment of electrical storm: a systematic review and meta-analysis. Sci Rep. 2024;14(1):24719.
- Nair A, Bhoi S, Choudhary Y. Cease the storm - Successful stellate ganglion block in terminating refractory electrical storm. Am J Emerg Med. 2024;81:160.e3-160.e7.
- Yokota S, Taneyama C, Goto H. Different Effects of Right and Left Stellate Ganglion Block on Systolic Blood Pressure and Heart Rate. Open J Anesth. 2013;3(3):143-7.
- Kirkpatrick K, Khan MH, Deng Y, Shah KB. A Review of Stellate Ganglion Block as an Adjunctive Treatment Modality. Cureus. 2023;15(2):e35174.
- Reinertsen E, Sabayon M, Riso M, Lloyd M, Spektor B. Stellate ganglion blockade for treating refractory electrical storm: a historical cohort study. Can J Anaesth. 2021;68:1683-9.
- Cardona XR, Butnaru DS, Ribero OF. G. Bloqueo De Ganglio Estrellado como una estrategia de manejo en cuidado paliativo en paciente con arritmias cardíacas terminales: Serie De Casos. Rev Chil Anest. 2024;53:66-72.
- Elmofty D. Ultrasound-guided blockade of the stellate ganglion offers precise anatomical targeting while minimizing unintentional puncture of vital structures and reducing local anesthetic volume. 2020. In ASRA News, August 2020. Accessed at https://www.asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2020/08/01/how-i-do-it-stellate-ganglion-blocks
- Ultrasound-Guided Cervical Sympathetic Block. Accessed at https://www.nysora.com/pain-management/ultrasound-guided-cervical-sympathetic-block/
- Tian Y, Wittwer ED, Kapa S, McLeod CJ, Xiao P, Noseworthy PA, et al. Effective Use of Percutaneous Stellate Ganglion Blockade in Patients With Electrical Storm. Circ Arrhythm Electrophysiol. 2019;12(9):e007118.
- Goel V, Patwardhan AM, Ibrahim M, Howe CL, Schultz DM, Shankar H. Complications associated with stellate ganglion nerve block: a systematic review. Reg Anesth Pain Med. 2019:rapm-2018-100127. Epub ahead of print
- Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018;72(14):e91-e220. Erratum in: J Am Coll Cardiol. 2018;72(14):1760.
- EM:RAP. Stellate Ganglion Block in VF. July 7, 2024. Source: https://www.emrap.org/episode/ep19/stellateganglio
- GANGlion Stellate Block for Treatment of Electric storRm (GANGSTER Trial). Institute for Clinical and Experimental Medicine. Source: https://ctv.veeva.com/study/ganglion-stellate-block-for-treatment-of-electric-storrm-gangster-trial
More Resources
Regional Anesthesiology and Acute Pain Medicine YouTube
CoreUltrasound

