
The Case for Identifying and Situationally Anesthetizing the Radial Nerve at the Mid Humerus Shaft: A Reproducible and Consistent Technique to Identifying the Radial Nerve
Brian H. Torres-Gonzalez, MD ¹
Judy Lin, MD, FPD-AEMUS ²
Daniel Puebla, MD ¹
Daniella Lamour, DO ¹
Robert Farrow II, DO, FPD-AEMUS ¹
¹ Mount Sinai Medical Center
² Baylor Scott & White All Saints
The world of regional analgesia has witnessed a significant revolution in recent decades, with the advent of ultrasound-guided regional analgesia (UGRA) offering a blend of precision, safety, and efficacy.1-4 Forearm nerve blocks have been demonstrated to be some of the most utilized and frequently adopted UGRA procedures in the emergency department (ED).4-6 Among these forearm nerve blocks, the radial nerve block stands out for its various approaches depending on the technique and desired regions of analgesia.7 Thus, a pivotal step in performing this UGRA procedure is determining the ideal location for identifying the nerve and the appropriate branch for blockage. Inconsistent anatomy and lack of a standard ultrasound technique for identification of the radial nerve and its various branches can lead to improper anesthetic placement and block failures. We suggest that the spiral groove along the mid-shaft of the humerus is an ideal sono-anatomic landmark for identifying the radial nerve. Targeting the radial nerve in the mid-humeral position offers several benefits as it allows for identification of the radial nerve prior to any significant bifurcation as well as the ability to correctly identify its various branches as the scan is continued distally.
In this context, the mid-humerus shaft is not just an arbitrary location in the arm's anatomy; it holds strategic significance. The radial nerve, the largest nerve in the upper extremity, arises from the posterior cord of the brachial plexus. From the axilla, it traverses along the posterior aspect of the humerus through the cubital fossa, continuing along the dorsal aspect of the forearm, where it bifurcates into the superficial and deep branches.8 When the radial nerve is along the posterior compartment of the arm, it remains relatively superficial and identifiable at the mid-humerus level, making it a prime spot for reproducible identification and possible anesthetic placement. On ultrasound evaluation, the radial nerve will appear as a honeycombed structure superimposed on the humeral cortex which is obvious as a hyperechoic structure with posterior shadowing. (Figure 1) If the same orientation is maintained while sliding the probe distally the radial nerve begins to branch with the deep branch extending between the brachioradialis and brachialis muscles. (Figure 5) We suggest that recognizing the radial nerve in the mid-humeral position may ensure a higher success rate for the UGRA procedure regardless of the final desired position for injection as it allows for easy identification of the radial nerve branches as the probe is moved distally along the arm. In the mid-humerus position, the radial nerve is within a deep fascial plane accompanied only by the profunda brachii artery that is adjacent to it. If the UGRA is performed here, careful injection into the fascial plane will assist in reducing the risk of arterial infiltration or injury. It is recommended to use an in-plane needle technique regardless of the final position chosen for injection for full needle visualization.
Beyond reliable identification of the radial nerve, another advantage to utilizing the mid-humerus shaft position for analgesia of the radial nerve is that a single injection can anesthetize the major branches of the radial nerve as well as the posterior and lateral sensory branches. Selectively blocking the superficial branch of the radial nerve allows for purely sensory blockade of the radial part of the wrist, dorsal hand, and radial half of the extensor surfaces of the thumb and ring finger.9 However, this area does not provide anesthesia of the posterior-lateral aspect of the forearm and will not have motor involvement. Similarly, a selective blockade of the deep branch of the radial nerve will only provide anesthesia of the interosseous membrane, the periosteum of the radius and ulna, as well as the extensor surfaces of the carpal joints.8 (Figures 2 and 3) The mid-shaft technique may lend itself to a more robust and reliable analgesic distribution which could prove useful in procedures that radial nerve blocks are commonly used for such as dislocation reductions or fracture management.10, 11 The greater area of sensory blockade provided by a mid-humeral injection may also prove useful for lacerations or abscesses that extend along the posterior forearm and distal lateral-posterior arm.
Despite these advantages, the mid-humerus approach to the radial nerve block has not been well described in the ED literature. It has however been described in anesthesiology literature as an effective means of surgical analgesia for outpatient surgical procedures of the upper extremity.12 As mentioned above, there are multiple conditions that present to the ED daily that may benefit from blockade of the radial nerve.11 A mid-humeral approach to this peripheral nerve block will likely only further its utility but there is still much-needed exploration of this analgesic technique in the emergency setting. Anecdotally, we have found that the mid-humerus position is at the very least an extremely useful sono-anatomic landmark for teaching as it is a reproducible and consistent landmark for identifying the radial nerve and its various branches prior to any UGRA procedure.
Step by step tracing of the radial nerve from mid-humerus to supracondylar level:
To identify the radial nerve in the mid-humerus position, have the patient in a seated position with the arm extended or held over the abdomen with the elbow flexed. Start with the probe placed transverse across the posterolateral mid-humerus and identify the radial nerve as a hyperechoic honeycombed structure lying directly on top of the humerus. At this point the radial nerve lies within the spiral groove and is also seen adjacent to the deep brachial artery. (Figure 7A)
Branches off the radial nerve that occur within the spiral groove from proximal to distal include: the posterior cutaneous nerve of the arm, motor branch to the lateral head of the triceps, motor branch to the medial head of the triceps and anconeus muscles, lower lateral cutaneous nerve of the arm, and the posterior cutaneous nerve of the forearm. The sensory distribution of these nerves in addition to the superficial branch of the radial nerve occurring below the elbow crease can be seen in Figure 7B. The osteotome distribution of the radial nerve and its branches is seen in Figure 7C.
As the probe is moved distally along the spiral groove, the posterior cutaneous nerve of the forearm can be seen branching from the radial nerve just prior to the lateral intermuscular septum (Figure 7D). In Video Clip 1, the radial nerve passes from the triceps into the biceps through the linear echogenic lateral intermuscular septum, which is a hyperechoic connective tissue layer separating the dorsal and anterior compartment of the arm.13
As the radial nerve is traced further distally, it can be seen leaving the spiral groove and wrapping around the anterior arm as it moves medially in between the brachioradialis and the brachialis muscle (Video Clip 2). The probe at this point is 3-4 cm above the elbow crease. This is the level that is blocked in the supracondylar UGRA. (Figure 5) A block at the supracondylar level will anesthetize the superficial and deep branch of the radial nerve as this branchpoint occurs distal to the elbow crease at the cubital fossa. The deep branch of the radial nerve continues between the brachioradialis and brachialis muscles, then passes through the supinator muscle emerging as the posterior interosseous nerve (PIN). The PIN provides motor innervation for the extensor muscles in the posterior compartment of the forearm as well as some sensory fibers to the dorsal wrist capsule. The superficial branch runs deep to the brachioradialis muscle then runs along the radial artery into the forearm, crossing over the snuffbox to the dorsum of the hand, and provides sensation to the dorsal hand and digits in the radial distribution.
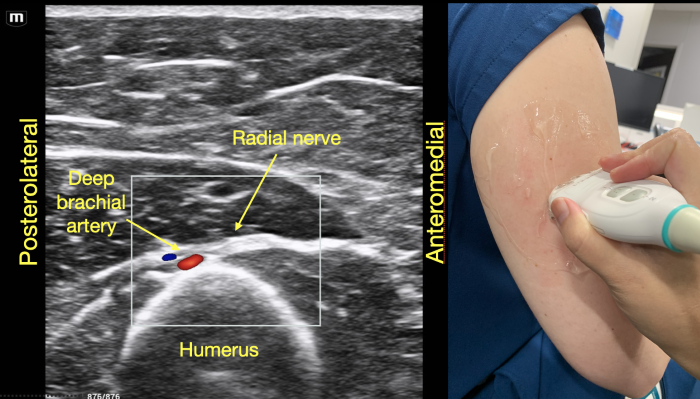 Figure 1. Radial nerve lying directly on top of the mid-humerus adjacent to the deep brachial artery.
Figure 1. Radial nerve lying directly on top of the mid-humerus adjacent to the deep brachial artery.
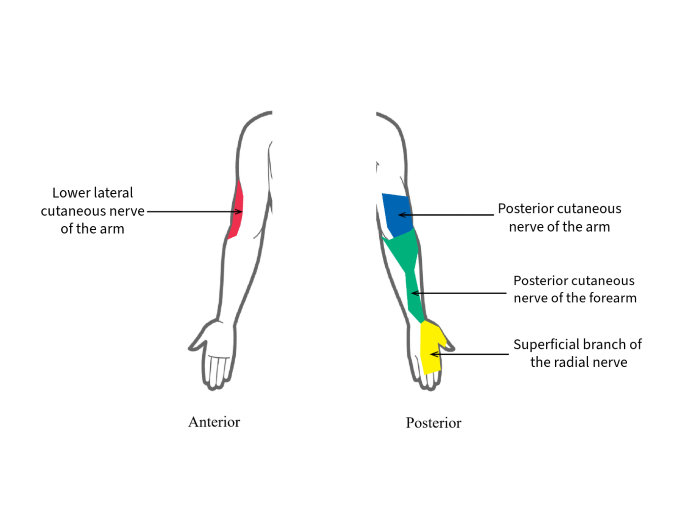 Figure 2. Sensory distribution of branches off the radial nerve
Figure 2. Sensory distribution of branches off the radial nerve
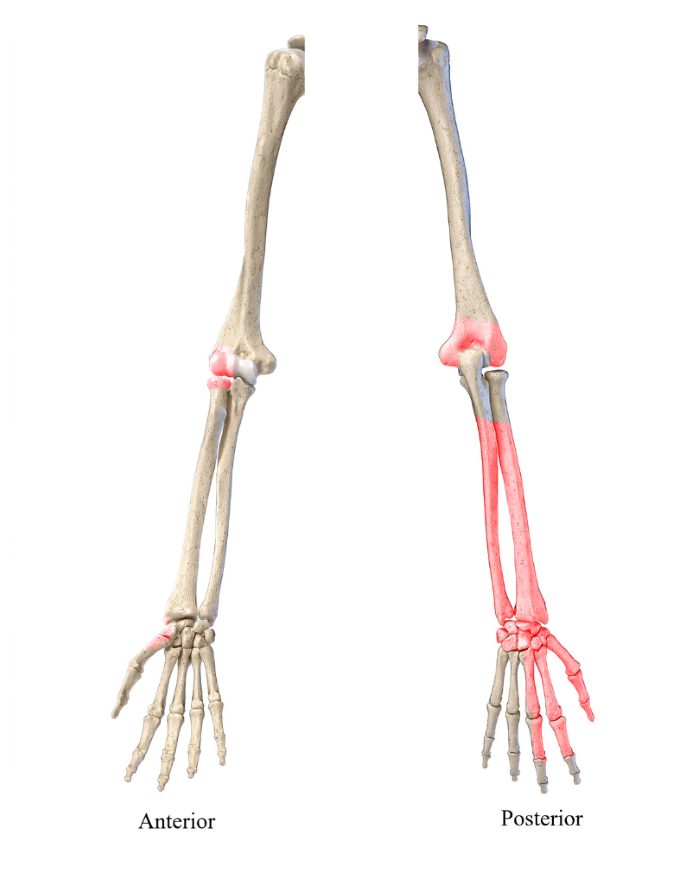 Figure 3. Osteome distribution of the radial nerve
Figure 3. Osteome distribution of the radial nerve
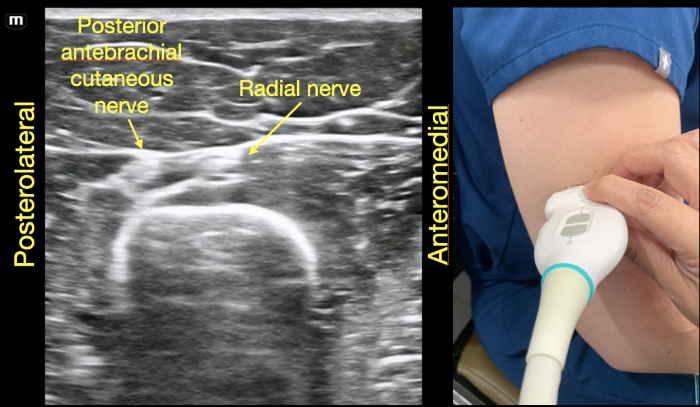 Figure 4. Posterior cutaneous nerve of the forearm branching off the radial nerve at the distal end of the spiral groove
Figure 4. Posterior cutaneous nerve of the forearm branching off the radial nerve at the distal end of the spiral groove
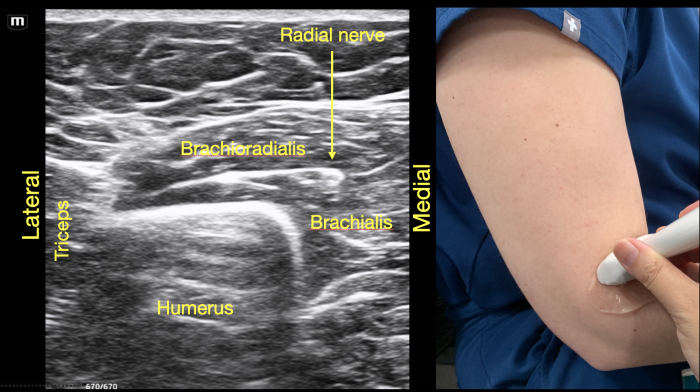 Figure 5. Supracondylar location of the radial nerve below the spiral groove
Figure 5. Supracondylar location of the radial nerve below the spiral groove
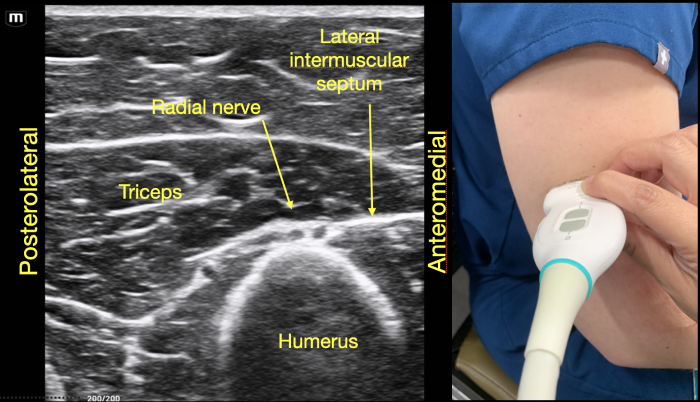 Figure 6. Radial nerve joins the posterior cutaneous branch of the forearm proximal to the lateral intermuscular septum in the dorsal compartment of the arm.
Figure 6. Radial nerve joins the posterior cutaneous branch of the forearm proximal to the lateral intermuscular septum in the dorsal compartment of the arm.
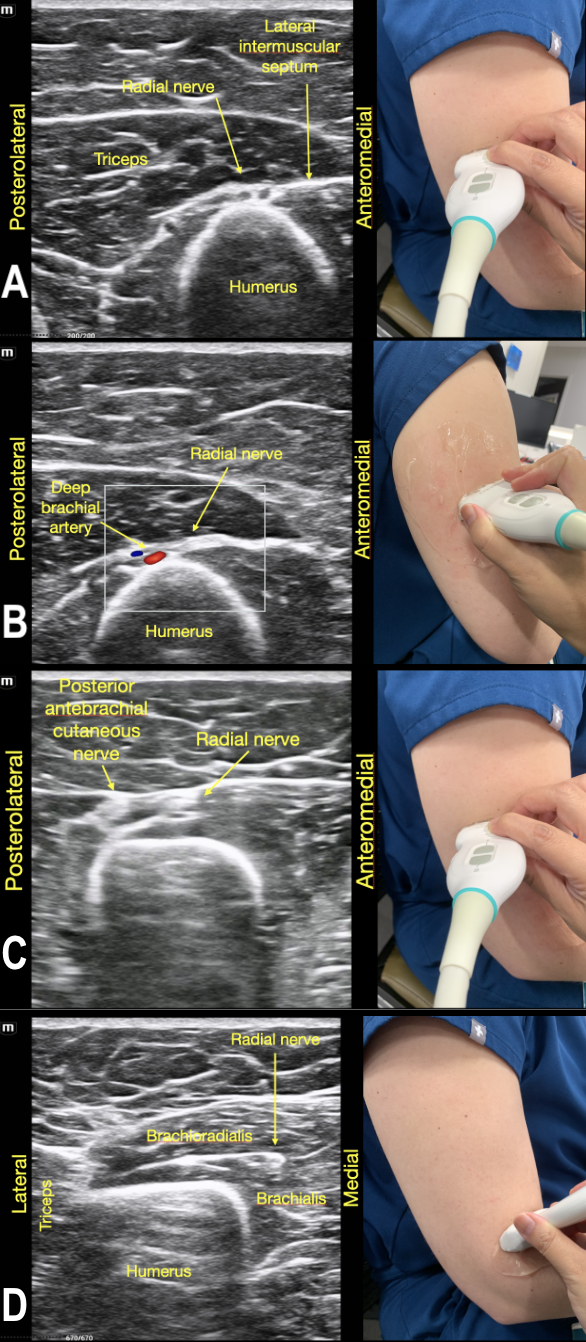 Figure 7. The Radial Nerve in its trajectory proximal to distal.
Figure 7. The Radial Nerve in its trajectory proximal to distal.
Video Clip 1. Proximal radial nerve in the spiral groove.
Video Clip 2. Distal radial nerve with bifurcation near the supracondylar position.
References
- Sites BD, Brull R. Ultrasound guidance in peripheral regional anesthesia: philosophy, evidence-based medicine, and techniques. Current Opinion in Anaesthesiology. 2006;19(6):630-9. doi:10.1097/aco.0b013e3280101423
- Gray AT. Ultrasound-guided Regional Anesthesia. 2006;104(2):368-73. doi:10.1097/00000542-200602000-00024
- Merz-Herrala J, Leu N, Anderson E, Lambeck A, Jefferson J, Sobrero M, et al. Safety and Pain Reduction in Emergency Practitioner Ultrasound-Guided Nerve Blocks: A One-Year Retrospective Study. Ann Emerg Med. 2024;83(1):14-21. doi:10.1016/j.annemergmed.2023.08.482
- Farrow RA, Shalaby M, Newberry MA, Montes De Oca R, Kinas D, Farcy DA, et al. Implementation of an Ultrasound-Guided Regional Anesthesia Program in the Emergency Department of a Community Teaching Hospital. Ann Emerg Med. 2024;83(6):509-18. doi:10.1016/j.annemergmed.2023.11.013
- Vrablik M, Akhavan A, Murphy D, Schrepel C, Hall MK. Ultrasound-guided nerve blocks for painful hand injuries: a randomized control trial. Cureus. 2021;13(10):e18978. https://doi.org/10.7759/cureus.18978.
- Malik A, Thom S, Haber B. et al. Regional Anesthesia in the Emergency Department: an Overview of Common Nerve Block Techniques and Recent Literature. Curr Emerg Hosp Med Rep. 2022;10:54-66. https://doi.org/10.1007/s40138-022-00249-w
- Foxall GL, Skinner D, Hardman JG, Bedforth NM. Ultrasound anatomy of the radial nerve in the distal upper arm. Reg Anesth Pain Med. 2007;32(3):217-20. doi: 10.1016/j.rapm.2007.02.006. PMID: 17543816.
- Anagnostopoulou S, Saranteas T, Chantzi C, Dimitriou V, Karabinis A, Kostopanagiotou G. Ultrasound identification of the radial nerve and its divisions. Is rescue nerve block at or below the elbow possible? Anaesth Intensive Care. 2008;36(3):457-9. https://link.gale.com/apps/doc/A188796901/AONE?u=googlescholar&sid=bookmark-AONE&xid=6182785f
- Aydin AA, Bilge S, Murtaza K, Aydin G, Cinar O. Novel technique in ED: supracondylar ultrasound-guided nerve block for reduction of distal radius fractures. Am J Emerg Med. 2016; 34(5):912-3. http://dx.doi.org/10.1016/j.ajem.2016.02.032
- Balaban O, Aydın T, İnal S, Yaman M. Ultrasound-guided Mid-humeral Radial Nerve Block Provides Sufficient Surgical Anesthesia at Hand Dorsum: A Novel Method and Report of Three Cases. Cureus. 2019;11(1):e3949. doi 10.7759/cureus.3949
- Frenkel O, Herring AA, Fischer J, Carnell J, Nagdev A. Supracondylar radial nerve block for treatment of distal radius fractures in the emergency department. J Emerg Med. 2011;41(4):386-8. doi:10.1016/j.jemermed.2010.11.043
- Sehmbi H, Madjdpour C, Shah UJ, Chin KJ. Ultrasound guided distal peripheral nerve block of the upper limb: A technical review. J Anaesthesiol Clin Pharmacol. 2015;31:296-307.
- García-Martínez J, Miguel-Pérez M, Pérez-Bellmunt A, Ortiz-Miguel S, Viscor G. The Course of Posterior Antebrachial Cutaneous Nerve: Anatomical and Sonographic Study with a Clinical Implication. Int J Environ Res Public Health. 2021;18(15):7733.

